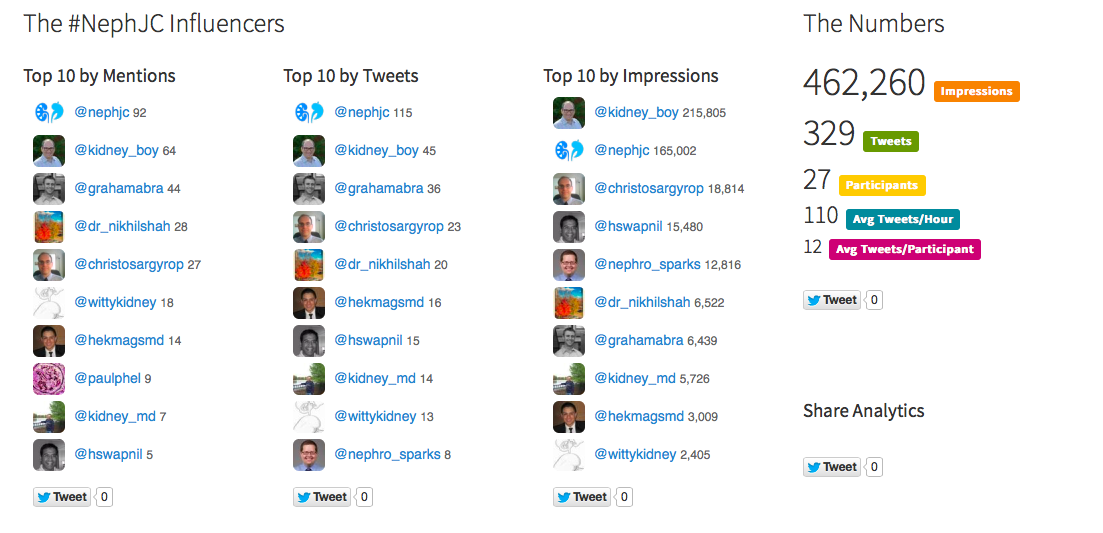
Tonight's and Wednesday's #NephJC is going to focus on the ACP guidelines. But it is important to recognize that a different group looked at the same data and came up with very different conclusions of what CPG should look like.
The American Urological Association Guideline (PDF) consists of 27 guidelines covering:
- Evaluation
- Diet therapy
- Pharmacologic therapy
- Follow-up
The AUA did consider 18 additional studies that were not part of the AHRQ analysis. The recommendations are graded and the authors interpreted the grades thusly:
- Clinical Principle. This is a statement about a component of care that is widely agreed upon by urologists or other clinicians for which there may or may not be evidence in the medical literature. My sense this is, that these recommendations are so woven into the fabric of stone care that people would not be able to get a study of these practices past an IRB.
- Expert Opinion. This is a statement, achieved by consensus of the Panel, based on clinical training, experience, knowledge and judgment for which there is no or insufficient evidence.
- A or B level evidence translated into Standards
- C level evidence becomes Recommendations
- Options are non-directive standards that may or may not be based on evidence. There is only one and it was evidence grade B
Background
- The prevalence of stones is increasing. It has gone from 5.2% in 1988-94 to 8.8% in 2007-2010.
- It is affecting more women so that it is much male dominated. The male:female ratio has slipped from 1.7:1 in 1997 to 1.3:1 in 2002.
- They looked at the diet studies that used stone formation as the outcome. Those studies found that increased water intake reduced stones. It found beneficial effect by avoiding cola.
- They looked at multicomponent diets and described the ability of a low sodium, normal calcium, low animal protein to reduce stones more than a low calcium diet.
- Two other studies restricted animal protein as part of a multicomponent diet and was unable to find any advantage.
- The authors point out that changes to urinary stone risk factors has not been validated as an intermediate endpoint.
The authors are transparent about one of the primary gaps in the use of diagnostic information about the nature of a stone in the therapy for that stone.
One caveat, all the RCTs diet studies were done in stone forming men.
The Guidelines
The 27 guidelines themselves are pretty straight forward and read like a description of what takes place in a well run stone clinic. The authors are again transparent, labeling many of the guidelines as Clinical Principle and Expert Opinion. In terms of the final score it looks like this:
Well over half the guidelines are opinion or clinical principle (which is just an opinion in a new hat).
Here is the breakdown by section:
Not surprisingly, only pharmacologic therapy has received significant RCT attention.
The AUA and ACP guidelines are based on the same evidence but ultimately look very different. The ACP guidelines look at this evidence desert and provide guidelines so sparse they end up functionally useless. The AUA, on the other hand, hitches the evidence to common sense, scientific innuendo, and long-held medical habit to provide fairly comprehensive guidelines that primary care doctors and part-time stone-physicians can use to actually take care of patients. The AUA guidelines paired with the AHRQ evidence analysis are documents I would have every fellow add to their iPad library. The ACP guidelines? Not so much.
In the end the ACP guidelines read like political statement protesting the sorry state of stone evidence, while the AUA guidelines provide a practical manual guiding stone care while still being transparent about the poor state of evidence.
Joel Topf, MD