#NephJC Chat
Tuesday April 25th 9 pm EST
Wednesday 8 pm BST, 12 noon Pacific
BMJ. 2017 Mar 9;356:j791. doi: 10.1136/bmj.j791.
Serum creatinine elevation after renin-angiotensin system blockade and long term cardiorenal risks: cohort study.
Schmidt M, Mansfield KE, Bhaskaran K, Nitsch D, Sørensen HT, Smeeth L, Tomlinson LA.
PMID: 28279964 (Paper free at BMJ)
Introduction
ACEs and ARBs are so familiar that I don’t even need to define their acronyms. The evidence for benefit from these drugs is so compelling that they now feature in the treatment guidelines for hypertension, heart failure, diabetes with albuminuria, CKD, and post-myocardial infarction care.
However, how we use ACEs and ARBs has changed. My most senior colleagues recall when patients were admitted to the hospital to start ACE inhibitors. Now these drugs are often subject to constant dose escalation and given as part of exacting multidrug regimens. As a result, the same guidelines that advocate their usage also suggest close monitoring and discontinuation if serum creatinine rises by 30% or more after starting treatment.
This week’s paper makes the points that very few patients receive the suggested monitoring, or discontinue therapy when they reach the suggested 30% creatinine rise criteria, which lacks firm evidence anyway. The paper therefore uses a retrospective population based cohort study to examine the relationship between cardiac and renal morbidity and creatinine rises after starting ACE/ARBs.
Methods
The authors used UK primary care databases to identify people over 18 years of age who started ACE/ARBs over a 17 year period and for whom pre- (up to 1 year before starting treatment) and post-initiation (up to 2 months after starting) creatinines were available. The outcomes of interest: time to ESKD, MI, new diagnosis of heart failure, and all-cause mortality were extracted from the same primary care databases as well as a raft of information about socioeconomic status, comorbidites and other medicines.
Results
The group found that 40% of subjects who started an ACE or ARB during the study period had pre- and post-initiation creatinine measurements (approximately 122,000 out of 303,000).
1.7% of patients had a creatinine rise over 30%, and of these “risers”, a higher proportion were female, had CKD 3B or 4, previous MIs, heart failure or peripheral vascular disease. “Risers” were also more likely to use loop diuretics, beta-blockers and NSAIDs. The blood pressure response after starting ACE/ARBs was similar, and socioeconomic status and diabetes did not differ between “risers” and “non-risers”.
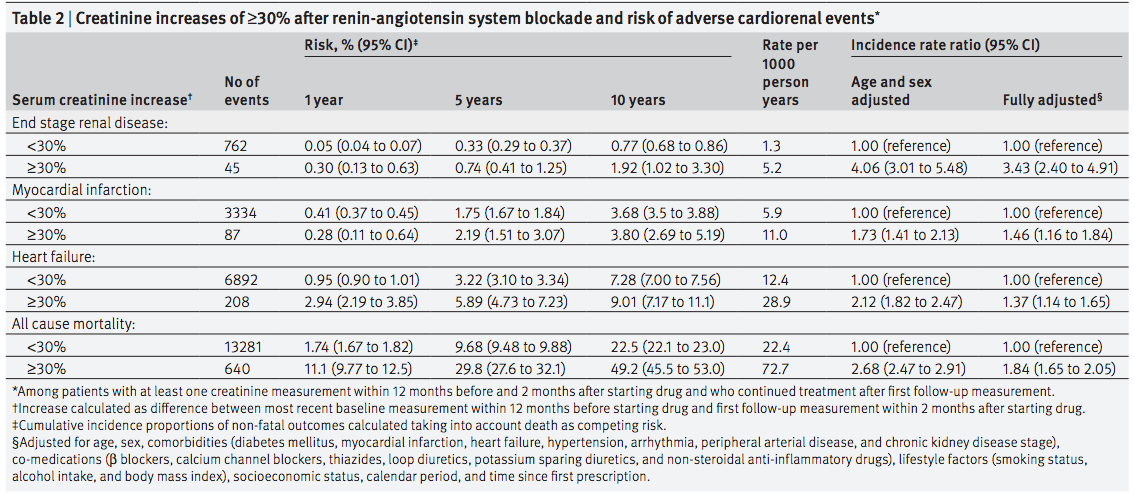
Increases in creatinine of 30% or more were associated with increased rates of all of the measured adverse outcomes. Although ESKD, heart failure and mortality all showed decreasing risk over time, there was a massive increase in incident rate ratio of 12.2 fold for ESKD in the first year and the risk persisted for 10 years. However, the event rate for ESKD was small and the confidence intervals were wide and heart failure and mortality showed much smaller effect sizes.
When the group examined the cumulative mortality according to creatinine increase after starting treatment, they found a dose-response relationship for creatinine rise that started when the creatinine rise was between 10-19% and persisted up to when it was over 40% (Figure 3). In addition, incidence rate ratios for ESKD, MI and heart failure also increased in a dose response relationship.
Take Homes
This study suggests that patients with a creatinine rise of 30% or more after starting an ACE or ARB are at increased risk of adverse outcomes and death.
The temporal data suggests that risks of adverse events are highest in the first year.
Categorising creatinine rises shows that increases in creatinine below the 30% level may also raise risk of adverse outcomes.
Strengths
Real world data
Size
Length of follow up
Weaknesses
Unable to adjust for proteinuria
Uncertain validity of ESRF and heart failure data in the databases
Only includes those who had pre and post treatment initiation creatinine measurements.
Discussion points
How much risk do creatinine rises under 30% confer to patients?
What is the true risk/benefit calculation of continued treatment versus discontinuation in all indications except heart failure now?
Do patients with pre and post start creatinine measurements represent the population as a whole? If not, could the population risk be different?
Can we really say that RCT data is more informative than these sorts of population cohorts?






Scintillating chats, very capably moderated by Joel and Francesco. From evidence based medicine full thermonuclear gif war!