North American Chat
GMT chat
Quite close - and the stats from Symplur don't capture all the differences. Very different feel, and discussion. Storify to follow.
Swapnil Hiremath, MD
This week, we will discuss whether less is more when it comes to discontinuing dialysis in patients with AKI and a chance to recover.
Holy Mackerel! This week we will discuss fish oil use in maintenance hemodialysis patients. Could this be the one thing that bends the curve on CV mortality, or is it just a red herring?
This week, we will discuss the phase 3 ORIGIN3 trial of atacicept, an APRIL/BAFF inhibitor for use in IgAN.
Day 3 of Kidney Week. Sibeprenlimab and Balcinrenone on NEJM and Lancet, plus a couple of other non-kidneywk studies.

North American Chat

GMT chat
Quite close - and the stats from Symplur don't capture all the differences. Very different feel, and discussion. Storify to follow.
Swapnil Hiremath, MD
A few months ago, we mentioned how to subscribe our feed with RSS.
At that time, we had one subscriber (Swapnil) - and to our great surprise, it seems to be that RSS is back. Just see below:

Unless there are spam RSS subscriptions somehow....
In some other news, we would like to thank Marjorie Lazoff for mentioning us in the LITFL blog - go check out their literature review here.
Swapnil Hiremath, M.D.
Tonight's and Wednesday's #NephJC is going to focus on the ACP guidelines. But it is important to recognize that a different group looked at the same data and came up with very different conclusions of what CPG should look like.
The American Urological Association Guideline (PDF) consists of 27 guidelines covering:
The AUA did consider 18 additional studies that were not part of the AHRQ analysis. The recommendations are graded and the authors interpreted the grades thusly:



The authors are transparent about one of the primary gaps in the use of diagnostic information about the nature of a stone in the therapy for that stone.


One caveat, all the RCTs diet studies were done in stone forming men.
The 27 guidelines themselves are pretty straight forward and read like a description of what takes place in a well run stone clinic. The authors are again transparent, labeling many of the guidelines as Clinical Principle and Expert Opinion. In terms of the final score it looks like this:

Well over half the guidelines are opinion or clinical principle (which is just an opinion in a new hat).
Here is the breakdown by section:

Not surprisingly, only pharmacologic therapy has received significant RCT attention.
The AUA and ACP guidelines are based on the same evidence but ultimately look very different. The ACP guidelines look at this evidence desert and provide guidelines so sparse they end up functionally useless. The AUA, on the other hand, hitches the evidence to common sense, scientific innuendo, and long-held medical habit to provide fairly comprehensive guidelines that primary care doctors and part-time stone-physicians can use to actually take care of patients. The AUA guidelines paired with the AHRQ evidence analysis are documents I would have every fellow add to their iPad library. The ACP guidelines? Not so much.
In the end the ACP guidelines read like political statement protesting the sorry state of stone evidence, while the AUA guidelines provide a practical manual guiding stone care while still being transparent about the poor state of evidence.
Joel Topf, MD
We are working on a survey of NephJC and I am trying to wrap my mind around what are the most important questions to ask. I really want to know how well NephJC compares as an educational experience to "In Real Life" journal clubs Thinking about that lead to this discussion on Twitter:
Some of the best NephJC discussions come after the hour long chat and can be off topic.
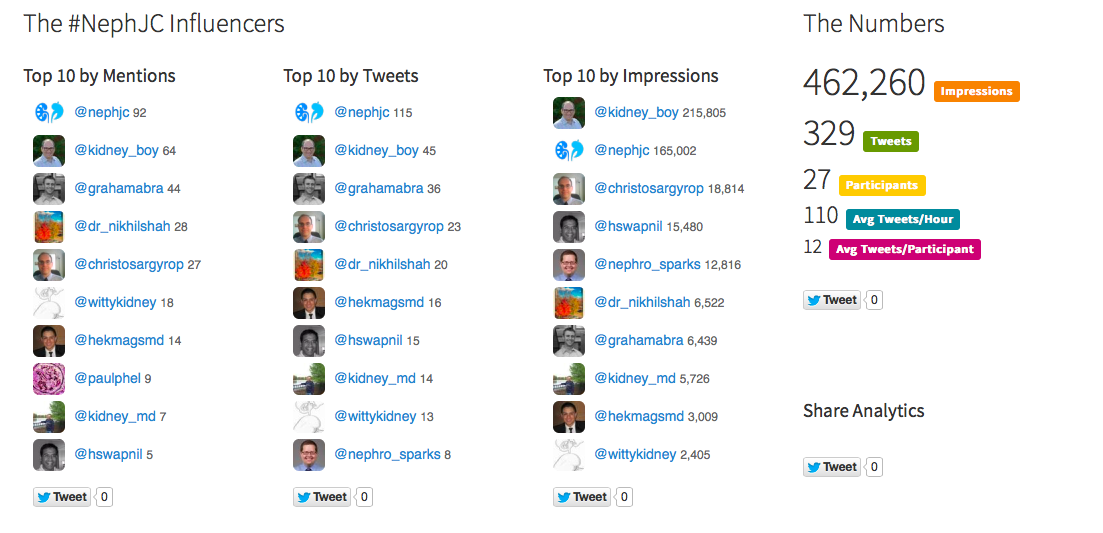
With a healthy bump in participants post #ERAEDTA15, just compare the participants. 'Nuff said.
The American chat

The GMT chat
As promised, the GMT chat storify is here, complete with the after party discussion on diuretics. Another superb curation by Hector!
Hector Madariaga - Nephrology Fellow from Syracuse and #NSMC intern - has now joined the #NephJC team. And you can see that why with the excellent job he has done with the storify of last week's chat. Watch this space for more contributions.
In case you were all wondering where the EU/African leg of the PD/CHF #NephJC chat disappeared, it will be held - albeit with a week's delay - on Wednesday June 3rd. It is all for a good reason. It has been quite busy for the Europeans this week - as you must have seen with all the furious tweeting from Charlie Tomson, Daniel McGuinness, David Arroyo, and many more including our very own Paul Phelan (who also wrote some excellent AJKD blog posts).

But, better late than never - and we hope many of you join us this week for the PD/CHF #nephjc chat.
Add this to the two articles by Alex Djuricich to flesh out your live-tweeting medical library.
You may have seen the evidence pyramid before, with animal studies and case reports at the bottom, and systematic reviews on the top.

Well, an interesting paper was published a few days ago, in the Journal of Medical Internet Research. Go ahead, click on that link and check it out.
It is a systematic review of all twitter-based journal clubs (and they seem to have captured all that were existing at that time). They have then examined the impact of these journals clubs using many different metrics. Interestingly, the one that immediately stands out is in table 2:

Table 2 from Roberts et al, http://www.jmir.org/2015/4/e103/
There's only one journal club with over a million impressions. Take a bow, all of you who have ever participated in a #NephJC chat!
The paper does make for interesting reading, apart from what we mention above. Some of the analyses agrees with our thoughts after the first dozen #nephJC chats.
The chat begins at 9PM EDT, in just an hour. The topics will be:
From the ASN Advocacy and Public Policy page:
If it wasn't from the pages of the New York Times I wouldn't believe it.
Please join us on #NephJC, Tuesday at 9PM EDT and Wednesday at 8PM GMT for a discussion of proper medical director behavior.
It was pretty well attended...

So was the GMT chat next day...

So our NSMC intern, Nikhil Shah not only did a super job of writing the sumary up for the BK virus #NephJC 22, he also has done a great job of curating the first chat into a storify.
The American chat (mostly by virtue of its longevity) still has more participants and tweets, but the GMT (EU/African) chat makes up by being fun and entertaining. Tom Oates, Paul Phelan, Francesco and their merry band of tweeters make for delightful reading. Jungle Juice, scud missiles and more. See some highlights below
@NephJC I never do EKG before starting quinolone, but always ask the patient: how long is your QTc? ;) #nephjc
— Fra Ian (@caioqualunque) March 4, 2015@ThePeanutKidney @NephJC Ideally when we use the untested jungle juice (cido,leflun,IVIg) we should do it as part of a study #nephjc
— Paul Phelan (@paulphel) March 4, 2015@swissnephro like the term PyVan 😄 pic.twitter.com/uA3wegSi1E
— John Booth (@ThePeanutKidney) March 4, 2015@NephJC nephrology's equivalent of a Scud missile - probably effective but lots of collateral damage #nephJC
— John Booth (@ThePeanutKidney) March 4, 2015March is Kidney awareness month and in honor of that, Pallimed, the Hospice and Palliative Care Blog is talking about intersection of nephrology and palliative care. They asked NephJC co-creator, Joel Topf to host their chat. This happens on Wednesday. Topf wrote the introduction:
Have you ever read a journal article and as soon as you finished the abstract you had this forbidding feeling that if the authors actually proved what they claimed to have discovered your medical life will never be the same?
This happened when I read, Functional Status of Elderly Adults before and after Initiation of Dialysis by Tamura et al. in 2009.
The study simply looked at mortality and functional status of nursing home residents who initiated dialysis. The cohort consisted of 3,704 Americans. The average age of this predominantly white (64%) female (60%) cohort was 74 years. The outcomes were horrifying:
While this study did not track patients who deferred dialysis it is hard to imagine they could do much worse. The view of dialysis as a way to improve functional status by clearing uremia leading to improved nutrition and other downstream benefits was revealed to be a false hope. Instead we have a treatment that appears to be too rough for frail, at-risk patients and left them significantly worse than they were before dialysis.
The discussion section of the article had a sentence that should be embroidered to every nephrologists white coat:
“...kidney failure may be a reflection of terminal multiorgan dysfunction rather than a primary cause of functional decline, and thus the initiation of dialysis may not rescue patients from an inevitable decline.”
As nephrologists we need to elevate conservative, non-dialytic, therapy to be a clear option for patients, one that should be discussed along with peritoneal dialysis and transplant. Conservative care should not merely be a last resort when all other options have been exhausted.
I hope you will join us as we discuss the intersection of nephrology and palliative care this Wednesday at #hpm chat.