#NephJC Chat
Tuesday March 12 2024 9 pm Eastern
Wednesday March 13 2024 9 pm IST
An update on the global disparities in kidney disease burden and care across world countries and regions
Bello AK, Okpechi GI, Levin A, Ye F, Damster S, Arruebo S, Donner JA, Fergus J, Caskey FJ, Cho Y, Davids MR, Davison SN, Htay H, Jha V, Lalji R, Malik C, Nangaku M, See E, Sozio EM, Tonelli M, Wainstein M, Yeung EK, Johnson DW; ISN-GKHA Group
PMID: 38365413
Introduction
Care of a patient with kidney disease extends far beyond the provision of renal replacement therapy. Comprehensive kidney care can include integrating pre-dialysis kidney care into existing health programs, enhancing patient and provider education on kidney care, and changing healthcare policies to improve access to kidney care. This is reflected in the ISN campaign theme for World Kidney Day 2024: "Advancing equitable access to care and optimal medication practice."
In celebration of this theme, NephJC will discuss the USRDS report and an article analyzing the current status of kidney care worldwide by the International Society of Nephrology - Global Kidney Health Atlas (ISN-GKHA). To understand this, we will briefly explore the development of ISN-GKHA over the past decade.
The ISN Global Kidney Health Atlas
Globally, over 850 million people are estimated to live with kidney disease, comprising more than 10% of the world's population (Jager et al, Kidney Int 2019). Despite the burden and health impact of kidney diseases, acute kidney injury (AKI) and chronic kidney disease (CKD) are often overlooked in major chronic disease control strategies. For instance, the World Health Organization's Global Status Report on Noncommunicable Diseases 2014 scarcely mentions kidney disease, hindering engagement with governments to address AKI and CKD.
"The first step in solving a problem is identifying one." Therefore, to address the issue of kidney disease, it's crucial to understand its burden. In 2016, the ISN launched the CKD 'Closing the Gaps' Initiative to provide a comprehensive strategy for addressing issues related to CKD care delivery worldwide. As part of this initiative, the ISN surveyed for the first time to assess the current state of global kidney care, covering AKI and CKD, and presented the results in a GKHA.
The initial report in 2017 highlighted kidney disease as a “silent epidemic”, and noted the general neglect of treatment and prevention strategies (ISN GKHA – 1st Edition). The second report in 2019 focused on the growing burden of kidney diseases and the significant regional inequities in access to treatments (ISN GKHA – 2nd Edition). The third report in 2023 illuminated the current capacity worldwide to deliver kidney care (ISN GKHA – 3rd Edition, 2023). Despite some observational studies and systematic reviews analyzing CKD burden, there remains a lack of comprehensive insight into the availability, accessibility, and affordability of kidney care worldwide, particularly in low-income and middle-income countries (LICs and LMICs). To address this knowledge gap, the current iteration of ISN-GKHA considers all CKD stages and analyzes the quality of care for people with kidney diseases, including renal replacement therapy (RRT) and conservative kidney management (CKM).
Methods
Desk research (literature review, kidney registries/databases) and opinion leader surveys were the two key methods used to produce the atlas. Additionally, patient surveys and support from local contacts and collaborators were also reviewed (Figure 1)
Figure.1. Data collection methods by ISN-GKHA
Peer-reviewed by the ISN executive committee, regional leaders, and international collaborators
Further reviewed by the ten ISN regional boards
Results were stratified by ISN region and World Bank country income group: LIC, LMIC, upper-middle-income country (UMIC), and high-income country (HIC)
Standard definitions were applied to components of renal replacement therapy (RRT), and conservative kidney management (CKM) based on established frameworks (USRDS, 2022 annual report; Davison et al., 2015, KDIGO)
Funding
The survey was funded by the International Society of Nephrology and its role was limited to providing administrative support for the ISN-GKHA design, implementation data collection, management, and submission of this report.
Results
Funding for Acute Dialysis and Renal Replacement Therapy
The global methods of funding for acute dialysis and KRT, which varied across regions and country income levels were described in Table 1 (very large table, not reproduced here, but check the paper for details). Important information is as follow:
Acute dialysis
For acute dialysis (either hemodialysis or peritoneal dialysis), reimbursement was covered by public funding (either free or with some fee at the point of delivery) in 63% of countries. It was more common in UMICs and HICs than in LMICs and LICs (Table 1).
Health system financing, publicly funded (free at the point of delivery) chronic hemodialysis was available in about half of the countries, ranging from 17% in North and East Asia and Oceania and South East Asia to 86% in Western Europe. The availability of funding increased as the income level of the country increased. In 32 (19%) out of 166 nations, public funding (with some costs at the point of delivery) for acute dialysis and chronic hemodialysis was accessible, mostly in North and East Asia. In Latin America, a mix of publicly funded and private systems prevails. Seven countries (4%) relied exclusively on private and out-of-pocket payments: the Democratic Republic of the Congo, Ghana, Madagascar, Nigeria, Tajikistan, Papua New Guinea, and Vanuatu (Table 1).
Chronic peritoneal dialysis
Reimbursement for chronic peritoneal dialysis was covered by public funding (either free or with some fee at the point of delivery) in 54% (90 of 166) of countries and was more common in UMICs and HICs than in LMICs and LICs. In almost all of Europe (Eastern, Central, and Western), there was government-funded access to peritoneal dialysis (free at the point of delivery); however, there wasn’t information in several countries and regions (Table 1).
Kidney transplantation
Public funding was available for kidney transplant recipients in 86 (52%) countries. Countries in Africa (40%; 16 of 40), Oceania and Southeast Asia (28%; five of 18), and South Asia (25%;two of eight) used solely private and out-of-pocket methods to pay for kidney transplant medications, while no HICs used this payment method. There are differences between regions (low-income to high-income) with respect to access to kidney transplantation by governmental agencies, but with some fees at the point of delivery (see Table 1 in the paper, which is too large to reproduce here).
Incidence and Prevalence
Data on the prevalence of chronic kidney disease was available in 161 (74%) of 218 countries, with a global median prevalence of 9.5% (IQR 5.9-11.7); this differs among different regions with 4.2% (3.5-5.2) in Africa to 12.8% (11.9-14.1) in Eastern and Central Europe. There were 94 (43%) countries with available data on the prevalence of treated renal failure; the range was from 4.4 cases pmp in Rwanda to 3679 cases pmp in Taiwan. The prevalence of treated kidney failure (median 823 cases pmp, IQR 556-11114) was over 200 times more in HICs than LICs. (Figure 2)
Figure 2. Global incidence (A) and prevalence (B) of treated kidney failure Bello AK et al. 2024
Of the 218 countries, 84 (39%) had data on the incidence of treated kidney failure; these were primarily HICs. The median incidence was 146 cases pmp per annum (IQR 107-213), with a range of 19 cases pmp in Ecuador and up to 529 cases pmp in Taiwan. The median prevalence of treated kidney failure was 823 cases pmp (IQR 556-1114) and was over 200 times higher in HICs compared to LICs. The following figure shows information on individual hemodialysis and peritoneal dialysis.
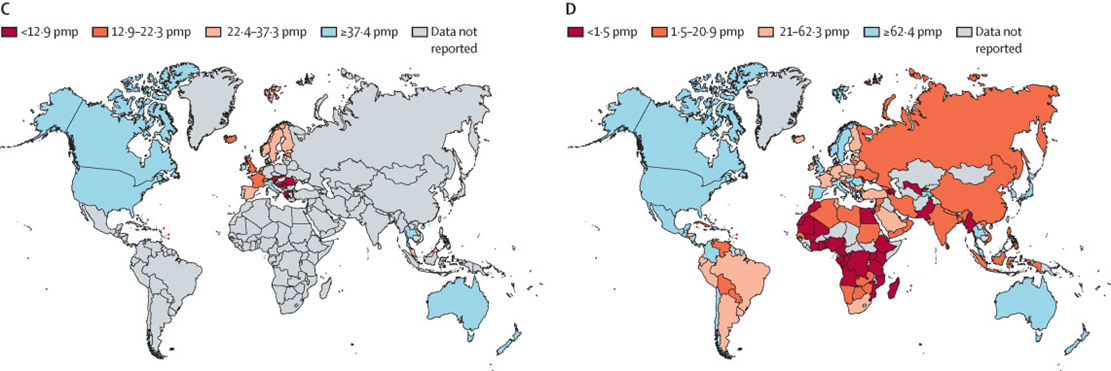
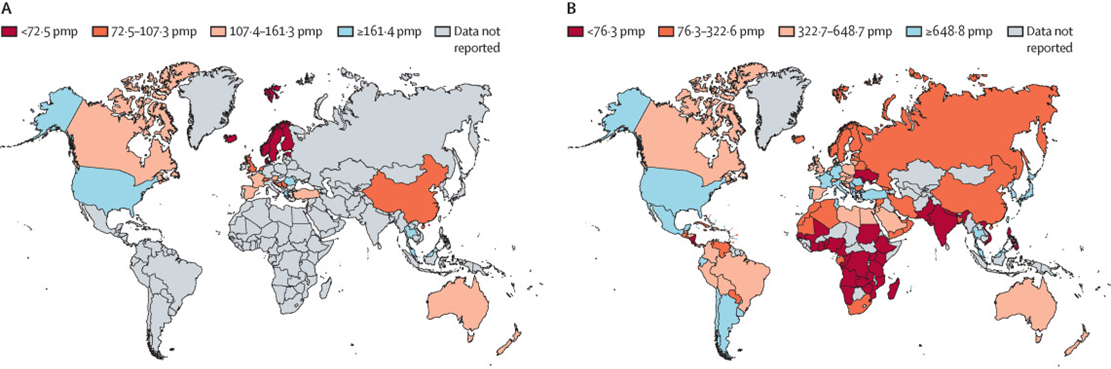
Figure 3. Worldwide prevalence of chronic hemodialysis (B) and chronic peritoneal dialysis (D). Bello AK et al. 2024.
Overall, median total health spending was $353 (costs in US dollars) per capita, with median government health spending of $216 per capita and median out-of-pocket health spending of $92 per capita.
Of kidney replacement therapies, the greatest economic burden was seen in the first year of kidney transplant with a cost of $26,903, varying across countries and regions. The annual median cost of in-center hemodialysis was $19,380 per person, with the maximum cost in Costa Rica being $103,443. With respect to peritoneal dialysis, the median annual cost per person was $18,959; however, the cost in low-income countries increased to a maximum of $ 300,644.
Appendix Table A3: Annual cost of kidney replacement therapy.Bello AK et al. 2024.
Overall densities per 1000 population of 36.2 nurses, 17.7 medical doctors, and 1.9 specialist physicians. There was significant variability in the capacity of RRT delivery across countries (Figure 4). The availability of hemodialysis (HD) centers was a median of 5.1 centers pmp (Figure 4A). In the case of peritoneal dialysis (PD) centers, the density was 1.6 centers pmp (Figure 4B). Availability of both PD and HD centers was lowest in Africa and highest in North America and the Caribbean. 49 countries, mostly HICs, provided home hemodialysis services.
Four of 130 countries provided acute peritoneal dialysis, 40 provided chronic peritoneal dialysis, and 86 countries provided both acute and chronic peritoneal dialysis. Automated peritoneal dialysis was available in 105 countries.
Figure 4. Availability of centers for hemodialysis, peritoneal dialysis, and kidney transplantation. Bello AK et al. 2024.
(A) Availability of centers for hemodialysis.
(B) Availability of centers for peritoneal dialysis.
(C) Availability of centers for kidney transplantation.
The median density of kidney transplantation centers was 0.46 centers pmp (Fig. 4C). Most countries (71%) had combined deceased-donor and living-donor kidney transplantation programs. Pediatric kidney transplantation was available in only 60% of countries.
Dialysis was accessible to more than half of people with kidney failure in 74% of the countries and varied by country income level, ranging from 19 (32%) in low-income countries to 62 (98%) in high-income countries. More than half of people with kidney failure were able to access dialysis in less than half of African nations (17 of 40 countries, 43%) versus Eastern and Central Europe, the Middle East, and North and East Asia where the dialysis was almost universally accessible.
Supplement Figure A2: Proportion of people living with kidney failure able to access dialysis Bello AK et al. 2024.
Conservative Kidney Management
Conservative Kidney Management (CKM), chosen through shared decision-making, was available in 53% (n=87 of 165) of countries, choice-restricted CKM was available in 65 (39%) of 165 countries, and choice-restricted CKM without resource constraints was available in 66 (40%) countries. The availability of CKM chosen through a shared decision-making process increased with country income level, but the availability of choice-restricted CKM did not. Infrastructure to support patients was available in 74 (45%) of 164 countries. Infrastructure to provide service delivery at home, a care home, or a hospice was available in 40 countries. Structures and processes for CKM delivery were available in less than 50% of countries worldwide.
Appendix Table A8a: Availability of structures and processes for CKM delivery Bello AK et al. 2024.
Essential medicine for pain and palliative care was available in 96 countries. In high-income countries, it is notable that a greater number of countries have access to infrastructure to document advance care planning conversations and provide psychological, social, and spiritual support (Appendix Table A8b).
Appendix Table A8b. Availability of essential medicines, infrastructure, and psychological support for CKM delivery Bello AK et al. 2024.
Vascular Access
Public funding (free, or with some fees at point of delivery) for central venous catheter placement was available in 96 of 166 countries. Public funding was available for vascular access creation (arteriovenous fistula or arteriovenous graft) in 89 of 166 countries, peritoneal dialysis catheter insertion in 88 countries, and kidney transplantation in 86 countries.
Healthcare Personnel
Data on the availability of healthcare personnel was available from 161 countries. In 145 out of 166 countries (87%), nephrologists were primarily responsible for the medical care of individuals with chronic kidney disease, while in 11 countries (7%), primary care physicians took on this responsibility. The global availability of nephrologists was 11.8 pmp (IQR 1.8-24.8). About one-third of all nephrologists were women. Globally, the median prevalence of pediatric nephrologists was 0·69 pmp (IQR 0·03–1·78). Reported shortages of kidney care providers were prevalent across several countries. For nephrologists, shortages were noted in 107 out of 167 countries (64%). Similarly, pediatric nephrologists were reported to be in short supply in 116 countries (69%), while transplant surgeons faced shortages in 109 countries (66%). Furthermore, shortages of dietitians were reported in 102 countries (61%), and dialysis nurses faced shortages in 97 countries (58%). These findings highlight a significant global challenge in ensuring adequate healthcare staffing for kidney-related care (Table 2 and Figure 5).
Table 2. Global distribution of medical kidney care workforce. Bello AK et al. 2024.
Appendix Figure A5. Shortages of healthcare providers essential for kidney care. Bello AK et al. 2024.
Mortality and morbidity in patients with kidney disease
Deaths from CKD ranged from 1.4% in the newly independent states and Russia to 5.5% in Latin America, with a median of 2.4% (IQR 1.56-3.9).
Supplement Table A1. CKD prevalence, DALYs attributed to CKD, and deaths attributed to CKD Bello AK et al. 2024.
For patients on hemodialysis, the most common reason for being hospitalized was infection in the vascular access used for dialysis. This was found in 32% of the countries. However, the leading cause of death for these patients in 77% of the countries was cardiovascular disease. For patients on peritoneal dialysis, the most frequent reason for hospitalization was peritonitis. This was seen in 51% of the countries studied. However, the main cause of death for these patients in 66% of the countries was also cardiovascular disease (Figure A8 and Figure A9).
Appendix Figure. A8. Causes of hospitalization among people treated with dialysis.Bello AK et al. 2024
Appendix Figure A9. Causes of death among people treated with dialysis. Bello AK et al. 2024.
Availability of registries across the world
In various countries, registries serve as vital databases for different stages of kidney disease management. Roughly 19% of countries maintain registries for chronic kidney disease patients who haven't yet progressed to requiring dialysis, while 63% track patients undergoing dialysis treatment. Additionally, kidney transplant data is recorded in 58% of countries, highlighting the global effort to monitor transplant outcomes. However, care for Chronic Kidney Disease Mineral and Bone Disorder is tracked in only 6% of countries, indicating a potential gap in monitoring this aspect of kidney health. These registries primarily focus on key aspects such as documenting incidents of kidney failure (89% of the time), the type of dialysis employed (95%), the method of access for dialysis (82%), and patient mortality rates (84%). However, there's variability in recording other crucial indicators, such as how effectively conditions like anemia or blood pressure are managed, or monitoring patient outcomes, which are not consistently tracked across all countries, indicating areas where improvements in data collection and monitoring could enhance kidney care globally.
Appendix Figure A6: Content coverage of dialysis registries. Bello AK et al. 2024.
Appendix FigureA7: Content coverage of kidney transplant registries.Bello AK et al. 2024.
A quarter of 162 countries had a chronic kidney disease detection program base on a national policy or guideline. However, a higher proportion was implemented via a reactive approach, through routine health encounters and specific screening processes. Less than half of countries had governments that overtly recognize chronic kidney disease as a health priority.
Chronic kidney disease hotspots were reported in 46 of 162 countries. The two main industries in hotspots were Agriculture and mining, and several traditional and environmental risk factors such as diabetes, hypertension, and contaminated water were identified (Table A12A).
Appendix Table A12A: Factors contributing to kidney disease hotspots. Bello AK et al. 2024.
The USRDS 2023 Annual Data Report
The United States Renal Data System (USRDS) 2023 Annual Data Report (ADR) contains updated information about the CDK and ESRD populations in the U.S. through the end of 2021. It also provides information about the second year of the COVID-19 pandemic.
Methods
From the report description, ‘The United States Renal Data System (USRDS) is a national data system that collects, analyzes, and distributes information about chronic kidney disease (CKD) and end-stage renal disease (ESRD) in the United States. The USRDS is funded directly by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). USRDS staff collaborate with members of the Centers for Medicare & Medicaid Services (CMMS), the United Network for Organ Sharing (UNOS), and the ESRD networks, sharing datasets and working to improve the accuracy of ESRD patient information.’ The USRDS was initiated in 1988, approximately 15 years after the actual establishment of the ESRD program and national coverage for dialysis across the United States. The push for establishing this was due to concerns of high morbidity and mortality with RRT (Port et al, AJKD 2019; Collins et al, KI Supplement 2015). It was funded by the NIDDK, with support from the CMMS. In addition to the report highlighting incidence and prevalence, additional special studies are included annually (e.g., vascular access, adequacy). The contract for collating the ADR is awarded every few years to different academic institutions (e.g., the University of Minnesota in the past and the University of Michigan presently).
The 2023 Report
Incidence and Prevalence
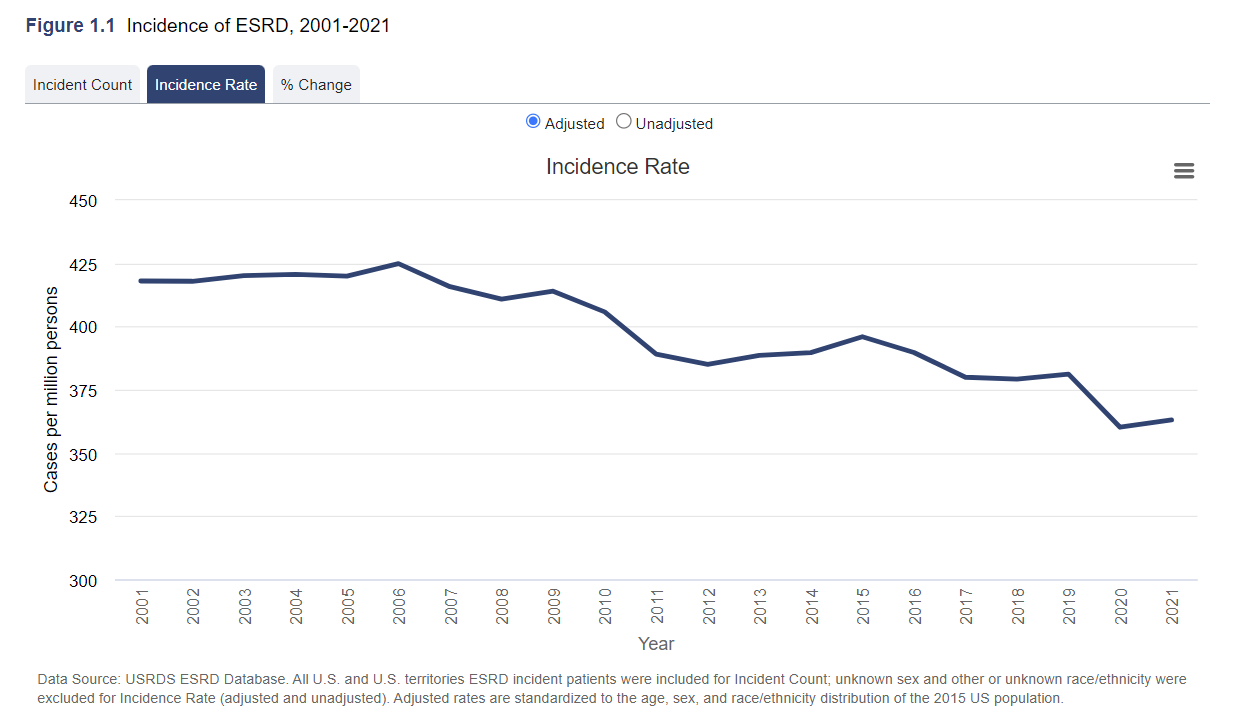
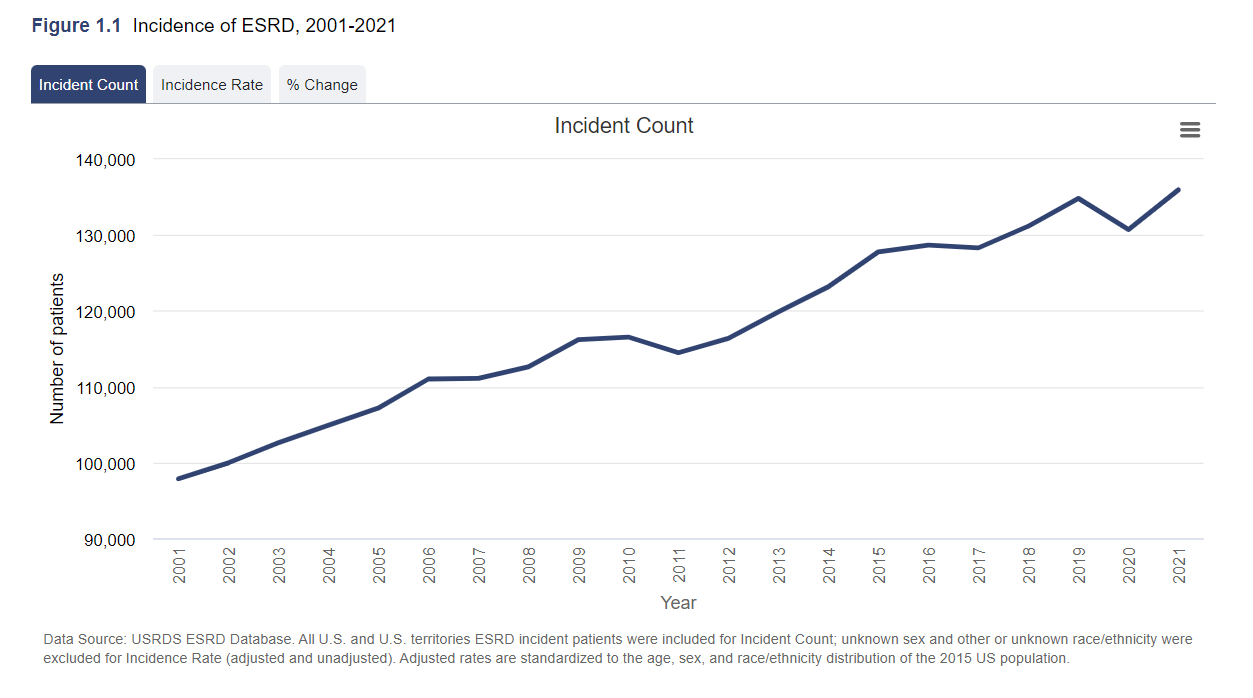
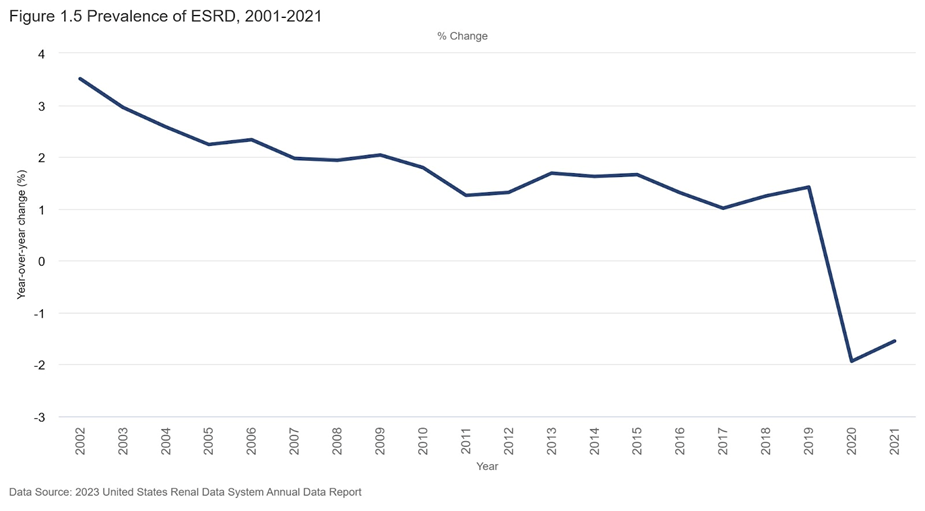
Patients with newly registered ESRD increased by 36,981 between 2001 and 2019. This indicates a 37.8% rise over time, possibly reflecting several factors, including the growing and aging population, higher rates of underlying diseases (such as diabetes) over time, and decreasing competing causes of death (e.g., decrease in cardiovascular mortality). However, the incidence rate (see below) has been decreasing at least since 2007. Possibly the effect of better blood pressure control, glycemic control, and renin-angiotensin system inhibitor use? Though flozination reduces risk of ESRD by 30-40%, this seems too early to see that effect. Additionally, the incidence count does keep increasing despite the decreasing incidence rate, due to the increase in the population. However, 2020 was the first year where the incidence count actually decreased - likely related to the COVID-19 pandemic, and it has since rebounded back in 2021.
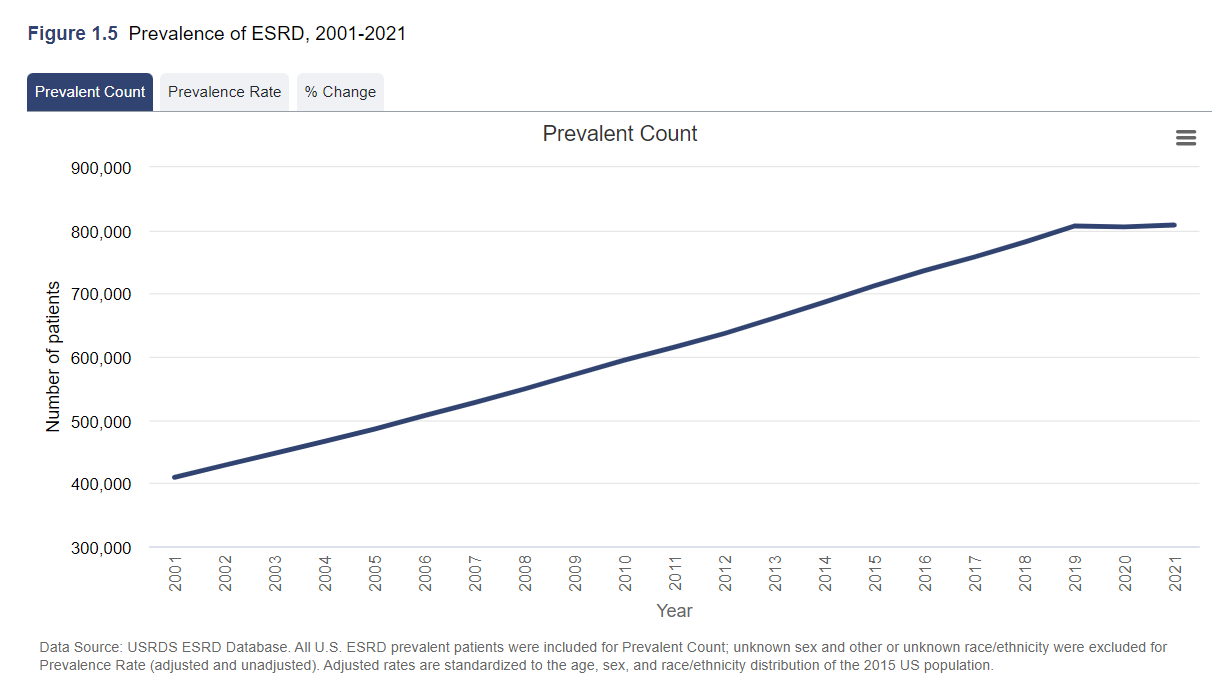
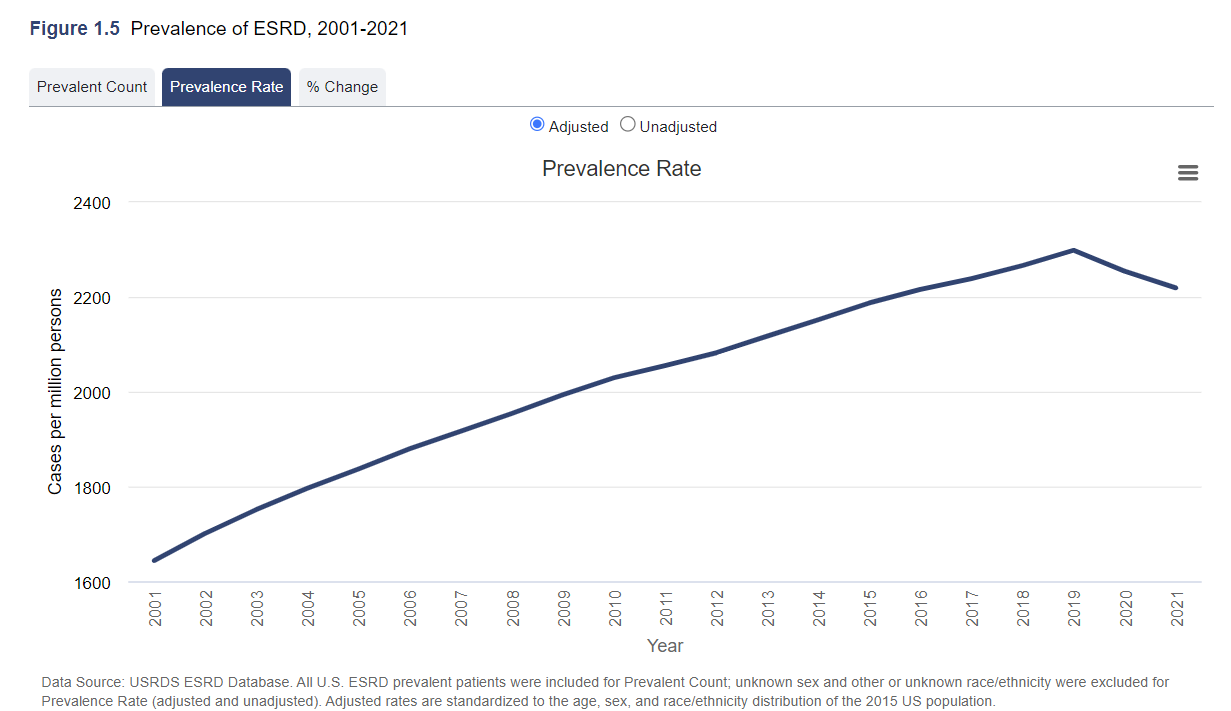
The change in incidence rate (top) and count (bottom) of ESRD, 2001-2021. United States Renal Data System. USDRS 2023
For the first time in 2020, there was a decrease in the number of individuals with prevalent ESRD with respect to 2019 (from 806, 939 to 806, 629), and ESRD prevalence to 2254 pmp. The prevalence of ESRD declined further in 2021 to 2219 pmp, a decrease of 3.5% since 2019. However, as noted in the below graph, the change in prevalence of ESRD was already declining, even before the pandemic and the more dramatic sudden drop. Hence, the prevalence count seems to have plateaued or possibly even declined, and the prevalence rate continues to decline. The prevalence numbers reflect the combined effect of lower entries into ESRD (i.e., lower incidence rates) and a heightened exit, especially in the last few years (higher mortality from COVID-19). The COVID-related mortality has decreased from the peak of 2020, and time will tell the net effects over the next few years of these risk factors.
Changes in prevalence of ESRD, 2001-2021; Absolute count (top) prevalent rate (middle) and percent change from year to year (bottom) .USRDS 2023
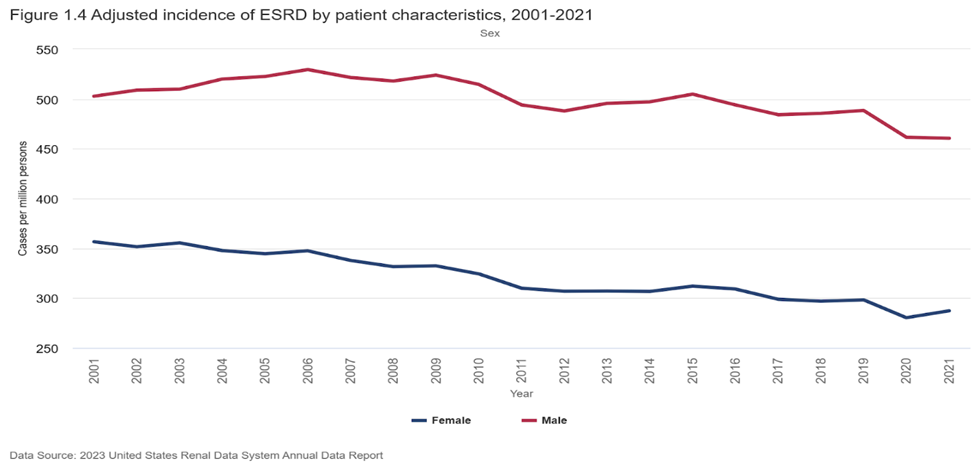
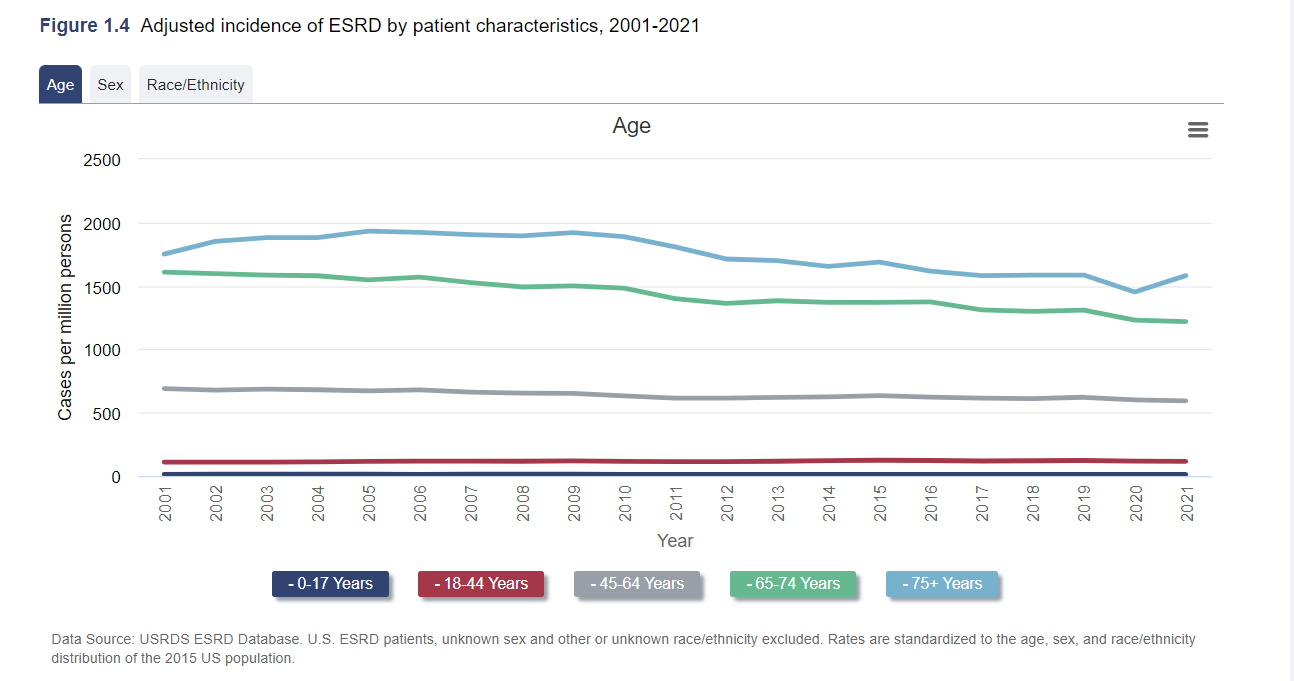
In 2021, the incidence of adjusted ESRD in men was 60.6% higher than that of women.
Adjusted incidence of ESRD by patient characteristics stratified by sex (top) and age (bottom), 2001-2021. United States Renal Data System. USRDS 2023
The adjusted ESRD incidence was higher among older age groups: in 2021, the adjusted incidence was from 12 pmp among individuals aged 0-17 years to 1581 pmp among individuals aged ≥75. Note the dip in the oldest age group in 2020, corresponding and contributing to the total incidence dip discussed above.
Until 2018 or 2019, the incidence of adjusted ESRD declined across all racial and ethnic groups. However, after 2019, the ESRD incidence has increased among Black individuals but not among other race/ethnic groups. In 2021, the incidence of ESRD among Black individuals was about twice as high as Hispanic individuals and four times as high as White individuals.
Adjusted incidence of ESRD by patient characteristics, 20001-2021.USRDS 2023.
ESRD Modality
The modality of kidney replacement therapy at ESRD onset in 2021 is shown in the following figure. A long way to go to reach the PD First goal (see NephMadness scouting report).
Modality at incidence of ESRD by patient characteristics, 2021. United States Renal Data System. USRDS 2023
It is observed that a higher percentage of older individuals initiated kidney replacement therapy with in-center HD (blue) compared with percentages-initiated PD (grey) or received a preemptive kidney transplant (green). Draws attention that home hemodialysis is not observed in the graph. When subanalysis was evaluated by gender and race, there were no salient differences between men and women. There were differences between Black and White individuals with respect to initiation of RRT to initiation of RRT with PD or a preemptive kidney transplant, this is higher in White individuals. The percentage using PD was highest among Asian individuals (20%), and the percentage who received a preemptive kidney transplant was highest among White individuals (4%).
This is just a snapshot of some of the data from the 2023 USRDS report - read the full report for much more in-depth information.
Discussion
In The Lancet Global Health, Bello and colleagues provide an update on the International Society of Nephrology Global Kidney Health Atlas, which evaluates kidney disease burden and care across nearly 191 countries (Bello AK et al. 2024). This comprehensive study, covering 97.4% of the global population, offers valuable insights into chronic kidney disease care capacity, including patients' perspectives, and aligns with WHO priorities for strengthening health systems and promoting universal health coverage. The authors need to be commended for this extensive data collection and evaluation. Based on extensive research and surveys, the report reveals a global median prevalence of chronic kidney disease at 9.5%. While hemodialysis services are nearly universally available, access to RRT remains limited, especially in low-income countries (LICs) and lower-middle-income countries (LMICs), as well as for children.
The incidence/prevalence rates for ESRD have been decreasing in recent years, according to data from the latest USRDS 2023 report. Collins et al.2011 reported that the USRDS documented a plateau and decline in incidence rates, a 28% decline in death rates since 2001. Besides, since then, it was observed that multidisciplinary care and the establishment of multidisciplinary CKD clinics lead not only to improved renal outcomes (i.e., stabilization of GFR and a delay in the initiation of replacement therapy) but also lower mortality, and create grounds for optimism (Batlle et al. Kidney Int 2006 and Ravani et al. J Nephrol 2003). Recently, the COVID pandemic increased the mortality and, consequently, decreased the prevalence count (Weinhandl. 2024).
The study highlights stark disparities in RRT costs, government health spending, and public funding for essential medications across countries. Interestingly, peritoneal dialysis is more costly in LICs than in HICs, contributing to poor outcomes in resource-poor settings where RRT is often unaffordable. Though labor costs are lower in LICs (thus decreasing the relative cost of HD), the consumables for PD are priced similarly due to the dialysis monopolistic companies (Baxter, Fresenius), which probably explains most of this discrepancy. Workforce shortages persist, particularly in LICs and LMICs, exacerbating the lack of services for managing CKD complications. Many regions lack national strategies and policies for kidney care, and barriers such as geographical constraints and economic factors further hinder access to care.
The findings underscore the urgent need for equitable access to kidney care globally, including preventive measures and early detection to reduce the burden of RRT. Sustainable strategies, including promoting transplantation and locally managed, cost-effective peritoneal dialysis, are essential for ensuring comprehensive kidney care. Advancements in CKD treatment, such as new drugs like SGLT2 inhibitors and finerenone, offer promising options to delay disease progression. However, ensuring access to these medications, particularly in low-income countries, remains a challenge. Workforce shortages persist, particularly in LICs and LMICs, exacerbating the lack of services for managing CKD complications. Finally, the study underscores the shift towards multidrug therapy in CKD management, suggesting the need for continued research.
Limitations
The study acknowledges potential biases, including social desirability bias, which may affect the accuracy of responses. The quantity and quality of literature on CKD in low-income and lower-middle-income countries are also relatively lacking.
The quality of RRT should be discussed, and the availability of modern treatments should be discussed. While some countries provide public funding for CKD care before RRT, this aspect is not extensively covered. Moreover, patient perspectives on RRT's impact on quality of life are minimally explored. Future iterations should expand on CKD care before RRT to address these limitations.
In Africa, the reported prevalence of CKD is lower than expected, given known genetic risk factors.
CKD complications contribute significantly to morbidity and mortality, a more comprehensive understanding of pre-RRT care is crucial.
Conclusion
In keeping with the theme of the 2024 World Kidney Day (Kidney Health For All), there's an urgent need to prioritize chronic kidney disease care globally, improve awareness, early detection, and management, and enhance access to essential medicines. Collaboration among medical specialties and advocacy efforts are essential for addressing this growing health concern.
Summary prepared by
Vamsidhar Veeranki
Assistant Professor, Nephrology
SGPGIMS
Lucknow, India
and
Elba Medina
Assistant Professor,
Hospital General de México "Dr. Eduardo Liceaga"
Mexico City, Mexico
NephEdC (NSMC) Interns, Class of 2024
Reviewed by Cristina Popa, Jade Teakell, Sabarinath,
Tiffany Caza, Brian Rifkin, and Swapnil Hiremath
Header Image created by AI, based on prompts by Evan Zeitler