#NephJC Chat
Tuesday Oct 30 9 pm Eastern
Wednesday Oct 31 8 pm GMT, 12 noon Pacific
Lancet. 2018 Jul 7;392(10141):31-40. doi: 10.1016/S0140-6736(18)31080-8. Epub 2018 Jun 14.
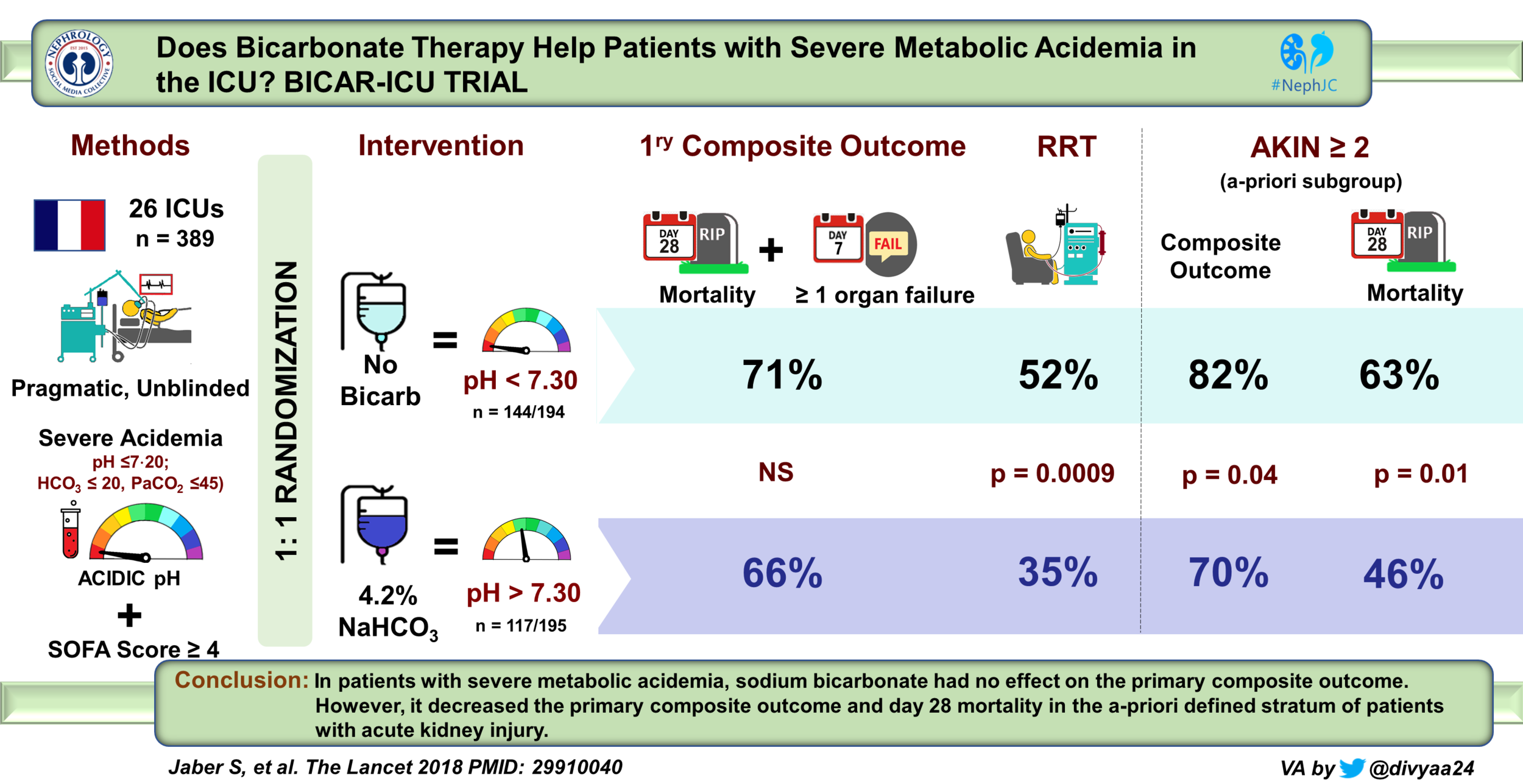
Sodium bicarbonate therapy for patients with severe metabolic acidemia in the intensive care unit (BICAR-ICU): a multicenter, open-label, randomized controlled, phase 3 trial.
Jaber S, Paugam C, Futier E, Lefrant JY, Lasocki S, Lescot T, Pottecher J, Demoule A, Ferrandière M, Asehnoune K, Dellamonica J, Velly L, Abback PS, de Jong A, Brunot V, Belafia F, Roquilly A, Chanques G, Muller L, Constantin JM, Bertet H, Klouche K, Molinari N, Jung B; BICAR-ICU Study Group.
PMID: 29910040 Full Text at the Lancet
PulmCrit Summary from Josh Farkas
Introduction
Metabolic acidemia is common in the critically ill intensive care unit (ICU) patient, and in the most severe cases (pH < 7.15 or 7.2), at some institutions, the standard of care is to give exogenous alkali to raise the pH (needless to say, the primary goal is always to correct the underlying etiology, so fixing the pH is only in addition to that goal). Theoretically, low pH causes poor cardiac contractility, increased arrhythmia, and vasopressor resistance. But does giving exogenous alkali fix that? Here is what the ‘Surviving Sepsis’ guideline from 2016 say:
“We suggest against the use of sodium bicarbonate therapy to improve hemodynamics or to reduce vasopressor requirements in patients with hypoperfusion-induced lactic acidemia with pH ≥ 7.15 (weak recommendation, moderate quality of evidence).”
the effect of sodium bicarbonate on clinical outcomes at any pH level, is unknown
Why would they do that? Well, giving bicarbonate is associated with sodium and fluid overload, an increase in lactate and PaCO2, and a decrease in ionized calcium. More worryingly, two trials reported no benefit from bicarbonate administration on vasopressor requirements or hemodynamics. Admittedly, these trials included few patients with a pH < 7.2. And there is little to no data on clinical outcomes. The guidelines continue, “the effect of sodium bicarbonate administration on hemodynamics and vasopressor requirements at lower pH, as well as the effect on clinical outcomes at any pH level, is unknown”.
More worryingly, administration of bicarbonate may paradoxically worsen intracellular acidemia. Have a look at this table from an excellent (though dated) review:
Table 1 from Forsythe and Schmidt, Chest 2000
Admittedly it’s animal data, but how else would you measure intracellular pH? The bottom line is that equipoise exists for the use of bicarbonate to treat the acidemia in these sickest of the sick patients.
Relevant to this debate are the pair of single center studies from last Spring, SALT-ED and SMART-ICU. These were discussed by NephJC. In these studies, balanced solutions reduced the risk of AKI compared to normal saline. One of the explanations was decreased non-anion gap metabolic acidosis with balanced solutions. A natural progression to this line of thinking of avoiding an acidemic state from fluid administration would be whether bicarb administration has any discernible benefit in the same population. Enter, stage left, the BICAR-ICU trial.
The Study
Methods
Study design
This was a multicenter randomized open label trial conducted in 26 ICU’s in France. To belabour the point, given that changes in pH would be easily observed by the treating team, this was an open label trial. However, computer generated allocation sequence was followed (ie allocation concealment was good). Additionally, randomization was stratified by three presecified factors: age with a cutoff of 65 years, presence or absence of suspected sepsis, and presence or absence of Acute Kidney Injury Network (AKIN) score of 2 or 3.
Inclusion Criteria
Age ≥18
Admission within 48 hours to ICU
severe acidemia pH ≤7.2 and PCO2 ≤ 45 and Bicarb ≤ 20
Total SOFA score ≥ 4 or LA ≥ 2 mmol/L
Exclusion criteria
Respiratory acidosis
Digestive or urinary tract loss of bicarb (volume loss ≥1.5L/day)
CKD 4
Ketoacidosis
Sodium bicarb infused (including initiation of renal replacement therapy [RRT]) within 24 hours before screening
Interestingly, a deferred consent model was used since the patients were unlikely to be able to consent + there may not be time to contact proxies in this situation. Hence permission was obtained at a later date.
Intervention
Patients were assigned in a 1:1 fashion to receive
either no bicarb or
IV sodium bicarb to maintain a pH >7.3. Bicarb concentration was 4.2% and the volume of administered bicarb was 125-250cc with a maximum of 1 L every 24 hours - and this protocol was followed through until 28 days or ICU discharge
In both groups, RRT was protocolized; strongly recommended at admission to the ICU if:
K >6.5 with EKG changes
cardiogenic pulmonary edema with or without urine production
At 24 hours after inclusion, RRT was recommended when two of the following were present:
urine output <0.3cc/kg/hour x 24 hours
Arterial pH < 7.2
K >6.5
Primary Outcome
A composite of
Death from any cause at 28 days or
Presence of at least one organ failure at 7 days
Secondary Outcomes
Use, duration of and number of days alive free from life support interventions (RRT, mechanical vent, vasopressors)
SOFA score at day 1, 2, 7 after enrollment
Total fluid intake between enrollment and day 2
Adverse events of electrolytes that occurred during ICU stay
pH>7.45
K >5 or <3.2
Na >145
iCa <0.9
ICU acquired infections
Length of stay in ICU
Analytic Plan and Sample Size
This was a superiority study, with an expected decrease in the primary outcome from 45% in control group to 30% in the intervention (bicarb) arm. For this, with 80% power, they would need 376 patients, which was bumped up to 400 to account for loss to follow up and consent.
The principal analysis was intention to treat (ITT);
Funding Source
The study was funded by the French Ministry of Health and the Société Française d’Anesthésie Réanimation.
Results
As planned, 400 patients were enrolled from about a 1000 potentially eligible. Only 11 did not consent, leaving 389 in the ITT analysis.
Figure 1 from Jaber et al, Lancet 2018
From table 1, these were around 60 years age, with about 80% being on a ventilator, requiring vasopressors, and 60% with sepsis. About half had AKI (AKIN stage 2 or 3).
Adherence was overall quite good at 88%; however this was different in both arms: 99% in the intervention group received bicarb, but 24% in the control group also received bicarb.
Primary Outcomes
In the overall population, bicarbonate infusion was not associated with an improvement in primary outcomes (organ failure at day 7 and any cause of death day 28) which occurred in 71% in control group and 66% in intervention (hazard ratio 0.78, p = 0.24). The survival at 28 days was 46% versus 55% (p = 0.09, shown below in figure 2A). After adjusted analysis however, sodium bicarbonate treatment was significantly associated with fewer deaths than control at day 28 (crude HR 0⋅78, ; p=0⋅091; and adjusted HR 0⋅73, p=0⋅0356).
There was no difference in length of ICU stay and days free from mechanical ventilation.
Figure 2A from Jaber at al Lancet 2018
Secondary Outcomes and Prespecified Subgroups
Figure 2C from Jaber et al, Lancet 2018
Thus in patients with AKI (AKIN score 2 or 3), bicarb arm resulted in a significant benefit in the primary outcome.
For secondary outcomes, there were some of interest:
Number of days alive and free from RRT was higher in the bicarbonate group vs. control group.
Number of days free from vasopressor was also higher in bicarbonate group
Infusion of sodium bicarb decreased need for RRT during ICU stay (52% vs 35% p .0009)
Figure 3 from Jaber et al, Lancet 2018
When RRT was indicated, it was started earlier in the control group.
More patients dependent on dialysis at ICU discharge in the control group than in bicarbonate group.
The reason for RRT was more likely to be acidemia and/or hyperkalemia in the control arm - versus more likely to be creatinine values in the bicarbonate arm.
From Supplementary appendix, Jaber et al, Lancet 2018
As expected, bicarbonate group had more metabolic alkalosis, hypernatremia, hypocalcemia
More interestingly, bicarbonate did indeed reduce potassium levels:
Discussion
Thus, though the overall results are negative, there was a benefit in the primary outcome in patients with AKI, as well as a benefit for renal outcomes overall.
As Josh Farkas points out, the investigators don’t differentiate the types of acidemia, and do these results suggest a greater benefit in uremic as compred to lactic acidosis?
The authors speculate that early sodium bicarbonate infusion might have bought time in patients with unstable severe metabolic acidemia and either avoided or delayed the initiation of the therapy in some patients.
An interesting point to note is the concentration of the bicarb fluid that was used in this study at 4.2%. For comparison a standard crash cart bicarb concentration is 8.4% in 50cc, and 3 amps of bicarb in D5W comes out to 1.3%.
Is this study enough to change practice, in critically ill patient with AKI?
Summary by Nimra Sarfaraz, Nephrologist, Dallas
NSMC Intern, Class of 2018
Banner image of Mono Lake, a Soda or Alkaline Lake, from Wikipedia by Brocken Inaglory, CC BY-SA 3.0