Long-term risks for kidney donors.
Mjøen G, Hallan S, Hartmann A, Foss A, Midtvedt K, Øyen O, Reisæter A, Pfeffer P, Jenssen T, Leivestad T, Line PD, Øvrehus M, Dale DO, Pihlstrøm H, Holme I, Dekker FW, Holdaas H.
PMID:24284516
North and South American #NephJC chat Tuesday Feb 3rd, 9 pm EST
Europe and Africa #NephJC chat: Wednesday Feb 4th 8 pm GMT
Introduction
“Living donor kidney transplantation is the preferred treatment for end-stage renal disease (ESRD).” So begins this week’s paper. If you are a nephrologist you have to believe this statement. Not only is live donation associated with better graft and patient survival, it also allows some patients with severe co-morbidities and complex immunological matching to receive a transplant they may not receive from a deceased donor.
Although donor nephrectomy is a safe operation in the immediate post-operative phase, long-term risk to the donor is less well characterised and assessment of this is the aim of this paper.
Methods
The authors sought to improve on previous live donor studies in two ways:
- They selected a control group that met criteria for kidney donation. Previous studies used the general population as the controls, which includes individuals unfit for donation. Making the control population sicker, hides potential morbidity associated with donation.
- Median follow-up of donors was 15.1 years, providing robust follow-up time to allow small differences in renal function to manifest.
The study followed-up 1,901 kidney donors and a control group of 32,621 individuals in Norway and captured data on death and progression to ESRD in the two groups. Donors and controls were well matched, however the donors were older.
Results
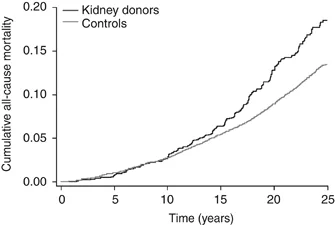
Figure 2 from article by Mjøen G et al, 'Long Term Risk for Kidney Donors" Kidney International (2014) 86, 162–167; doi:10.1038/ki.2013.460
- Mortality: Donors had an increased risk of death during follow-up, hazard ratio (HR) of 1.3 for all-cause mortality, and 1.40 for cardiovascular death.
- ESRD: HR for ESRD in donors was 11.38 and all those that developed ESRD were family members of the recipient. Median time from donation to ESRD was 18.7 years and 7 out of 9 donors who progressed to ESRD had an immunological cause of renal failure
Conclusions
So, in the words of the authors, this study “demonstrated a significant increase in ESRD, cardiovascular, and all-cause mortality during long-term follow-up after living kidney donation compared with a selected population of non-donors who would have met the criteria for donation.”
My take
With regards to death, we have known for some time that reduced renal function is associated with higher all-cause and cardiovascular mortality in general populations. Therefore the HRs for death are perhaps not surprising. When you add in the fact that donors may develop higher BP and low level proteinuria, and that both of these things also enrich mortality in the general population, then increased mortality could almost be expected.
On the subject of ESRD, the paper suggests this is more common in donors than health-matched controls with both kidneys in situ. The immunological component of ESRD in this study is particularly interesting when looked at in concert with a similar recent study in a US cohort. This US study showed that black donors were at particularly high risk of development of ESRD thus perhaps suggesting an underlying genetic component of progression in both cohorts.
NephJC summary written by Tom Oates (@toates_19) , winner of the best tweeter award from #KidneyWk14, and host of the European/African #NephJC chats.
Suggestion for Further Reading:
For those who want a nice review of the overall topic and direction it is heading, a post by Paul Phelan (@paulphel) on Renal Fellow Network is also worth perusing.
Join us on Tuesday Feb 3rd 9 pm EST or Wednesday Feb 4th at 8pm GMT for the next #NephJC discussion.