Infographic by Priti Meena @Priti899
Freely Filtered
Don’t miss Filtrate discussing the Top Nephrology Stories of 2021.
10. AKIKI2: There is Such a Thing as Too Late HD in AKI in The Lancet
post by Joel Topf @kidney_boy
In the last few years we have seen a steady drum beat of manuscripts dedicated to the hypothesis that starting kidney replacement therapy (KRT) in acute kidney injury early will improve patient outcome. And the consensus from IDEAL-ICU, AKIKI (NephJC summary), and STAART-AKI has been a resounding, “No.” So the authors of AKIKI-2 took those results, turned them around, and asked, “If starting KRT early doesn’t improve outcomes, can delaying the start of KRT as long as possible improve, or be neutral for patient outcomes?” The key to asking this question in a clinical trial is to really push the delay as long as possible. In AKIKI 2 patients could not be randomized until they had three days of oliguria or anuria or a BUN over 112. From there patients randomized to standard care would be started on KRT immediately and people in the delayed group would not receive kidney replacement therapy until their BUN was > 140 for a day. While the number of KRT free days (the primary outcome) did not differ between groups, there was a statistically significant increased risk of death with the delayed strategy. So delay KRT as long as possible, but not longer than possible.
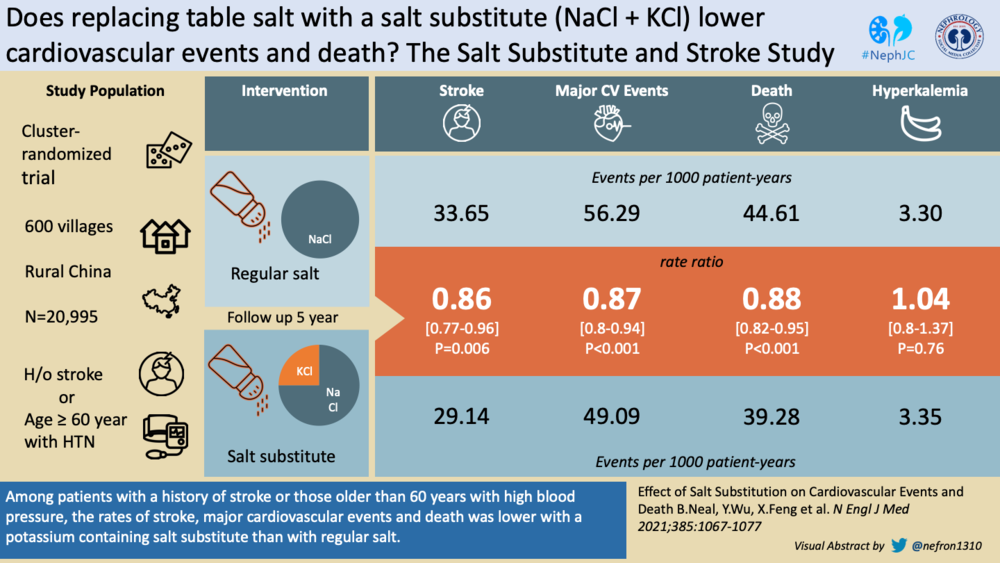
9. SSaSS: Potassium Salt In HTN Reduces Stroke and Mortality in NEJM
post by Sudha Mannemuddhu @drM_sudha
SSaSS study is an open-labeled cluster-randomized controlled trial conducted in rural Chinese population >/= 60 years old with hypertension or has a history of stroke that studied the effect of salt substitute (75% sodium chloride and 25% potassium chloride) compared to use of regular salt (100% sodium chloride) in decreasing cardiovascular events and death. And, oh boy, it did. In a 5-year follow-up period, stroke, major cardiovascular events, and mortality per 1000 patient-years were lower in the salt substitute group. Hyperkalemia was not an issue. The beauty of this study is that it not only proved that increased potassium intake is beneficial as shown in previous studies but also demonstrated effective implementation in day-to-day life, which is a major drawback with most ‘feeding studies’, where application ends after the study period. Randomization, low-cost intervention and long-term follow-up are some additional strengths of the study. Limitations with this study are the possibility of incomplete adherence, open-label, exclusion of population with ‘serious renal impairment’ etc. Though this intervention might not be applicable in most of the western world where foods are already salted or in those populations that do not / cannot prepare food at home, its ease of implementation, affordability, and more importantly, the possibility of decreasing the incidence of stroke is truly promising.
8. AURORA Trial (voclosporin) for Lupus Nephritis in The Lancet
post by Michelle Rheault @rheault_M
New effective drugs in nephrology should be celebrated and shouted from the rooftops, thus it is fitting that the AURORA trial landed in the 8th spot this year for Top Nephrology Stories. This study was a double-blind, placebo-controlled, randomized clinical trial testing whether the addition of voclosporin to standard treatment of lupus nephritis in adults would improve the proportion of patients achieving complete remission. The authors reported 41% of voclosporin treated patients achieved complete remission at 52 weeks compared to 23% of placebo treated patients (OR 2.65, CI 1.64-4.27, p <0.0001). Adverse events were similar in both groups. Why use voclosporin if other calcineurin inhibitors are already available? One major advantage is that voclosporin does not require trough drug level monitoring which makes it much easier for patients and physicians. One downside is the very high cost. While this drug will not change the world (there were still 59% of treated patients who were not in complete remission), it is another option for our patients with lupus nephritis who may not have responded to standard therapy. We’re looking forward to the completion of the followup AURORA2 study looking at 2 year outcomes for a possible #NephJC in the future.
7. FIGARO Completes the Finerenone Orchestra (CV Outcomes in DKD) in NEJM
post by Mohamed Elrggal @M_Elraggal
In 2021, finerenone came closer and closer to the hearts (and kidneys) of nephrologists and cardiologists. After FIDELIO (NephJC summary), the FIGARO-DKD trial tested the cardiovascular outcomes of finerenone in patients with kidney disease and type 2 diabetes mellitus (T2DM). While FIDELIO focused on patients with stage 3 or 4 CKD with frank albuminuria and T2DM (more advanced CKD), FIGARO enrolled patients with T2DM and either stage 2 to 4 CKD and moderately elevated albuminuria, or stage 1 or 2 CKD and severely increased albuminuria (earlier CKD stages). The primary outcome was cardiovascular; a composite of death from cardiovascular causes, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for heart failure. During a median follow-up of 3.4 years, finerenone reduced the risk of composite cardiovascular outcomes (by 13%) driven mainly by reduction in hospitalization for heart failure (by 29%). The study did not meet its secondary composite kidney endpoints, namely kidney failure, a sustained eGFR decrease of at least 40%, or renal death, however, finerenone decreased progression to ESKD. Finerenone did cause slightly more hyperkalemia with a rise in the use of K binders in the active group, and 1.2% hyperkalemia-related discontinuation of the drug (it should be noted that a run-in period actively maximizing RAS inhibition was used). While only around 8% of patients were receiving either an SGLT2 inhibitor or a GLP1R agonist at baseline, there were no worrisome signals of the combination. We are looking forward to FIND-CKD (finerenone in patients with CKD without DM), and FINEARTS-HF (finerenone in patients with symptomatic heart failure) trials. Finally, trials combining SGLT2i/GLP1R agonists and finerenone are much awaited with expected additive cardioprotective and nephroprotective effects, and also reduction of drug related adverse events like hyperkalemia (lower in SGLT2 inhibitor users).
6. Successful Genetically Altered Pig Kidney Transplanted into Human
Post by Swapnil Hiremath @hswapnil
Xenotransplantation: the final frontier. Think about it: if we could get a kidney from a live, albeit non-human donor, and it functioned, the transplant waitlist is no longer a waiting list. Dialysis could disappear as a modality of treatment in end stage kidney disease. The cynic scoffs at this stage as a cheap science fiction idea popularised in novels, as we have been down this road before. Baby Fae was the most famous of course, who lived with a baboon heart for a short 3 weeks in the early 80s. Even before that, in the 1960s, chimpanzee kidneys were famously transplanted, with one lasting for about 8 months. 5 decades later, the accumulation of scientific progress, including our understanding of xenobiology, immunology and the development of CRISPR has resulted into breaching the final frontier. On September 25th 2021, surgeons in New York transplanted a genetically modified pig into a neurologically dead patient. The organ was kept outside the body, and produced urine for at least 54 hours, and the urine did contain creatinine. The genetically modified kidney was from a pig from Revivicor, and we know from the news story that the alpha-gal gene was knocked out. Humans lack alpha-gal and quickly produce antibodies to reject organs otherwise, so this is key. Additional aspects include other xeno-antigens, as well as porcine endogenous retroviruses (PERVs) (see this CJASN review for an excellent overview) and another group has demonstrated in the past the ability to knock out the 62 PERVs with CRISPR. If this works out (and note that all we know about this breakthrough is from news stories), who should get these organs? What ethical issues are there? (PETA has an opinion of course) and will religion be a barrier to the use of pig organs? We do use porcine valves, corneas - and all the heparin we use for dialysis comes mostly from pig intestines. Those problems, along with the other surgical and immunological problems do need to be surmounted. For now, let’s celebrate that xenotransplantation is one huge step closer to becoming a reality.
5. KDIGO BP 2021 Update: 120 For All
post by Krithika Mohan @krithicism
KDIGO updated its BP guidelines a decade after its previous one and the magic number is 120. How? And how low? is the essence of the 2021 guideline. The 5 chapter guideline mainly emphasizes the need to standardize BP measurements and lowering BP targets in patients with CKD (not on dialysis). The KDIGO 2012 guideline made no recommendations on how to measure BP, simply because of lack of evidence. With more and more RCTs coming up, KDIGO 2021 incorporated the preparation and measurement techniques that contribute to an accurate BP reading-thus “Standardizing” the procedure. The KDIGO 2012 recommended a target of ≤140/80 or ≤130/80 mm of Hg if albuminuria was present. Shortly after, 2 major RCTs- SPRINT demonstrated cardiovascular and survival benefits and ACCORD showed decreased risk of stroke when the target SBP was ≤120 mm of Hg. KDIGO 2021 thus recommends aiming at a SBP of ≤120 for all patients with CKD irrespective of albuminuria/proteinuria (exception being patients on dialysis and kidney transplant recipients) - that is if the BP measurement was obtained in a standardized manner. It also recommends a slightly higher target in kidney transplant recipients- SBP≤130 mm Hg and DBP≤80 mm Hg due to lack of evidence of a stricter target and the possible risk of dramatic AKI and graft loss. The guideline also addresses the need for lifestyle interventions to lower BP in CKD while also emphasizing that the DASH diet and potassium based salts may not be appropriate in advanced CKD. In children, KDIGO stands its ground on lowering 24-hour mean arterial pressure (MAP) measured by ambulatory blood pressure monitoring (ABPM) to ≤ 50th percentile for age, sex, and height. Annual ABPM (if unavailable - use standardized auscultatory office BP) followed by 3-6 monthly standardized auscultatory office BP monitoring is recommended thereafter. Lastly, RAS inhibitors are recommended as the first line antihypertensive in patients with CKD of all age groups (in addition to calcium channel blockers in patients with kidney transplants). Overall, the take home message is to standardize BP measurement and achieve a target SBP ≤ 120 mm Hg (with exceptions of course!). Check out the NephJC summary for in-depth coverage of the guideline.
4. CLICK: Chlorthalidone Reduces BP in CKD in NEJM
post by Joel Topf @kidney_boy
In lecture after lecture for years the common wisdom was that thiazides are good diuretics, but when the eGFR slips below 30 or so, they should be shelved for their muscle-bound cousins, the loop diuretics. If you tried to find data to support this common wisdom you would be shut out, but an often referenced pilot study from 2014 did shine a light on the contrarian view, that chlorthalidone could be effective at low GFRs. Then at The Late Breaking, and High Impact Trials session of Kidney Week 2021, Dr. Rajiv Agarwal dropped CLICK (NephJC Discussion), a carefully conducted randomized controlled trial of chlorthalidone in advanced CKD for patients with uncontrolled hypertension. CLICK showed that modest doses of chlorthalidone on top of standardized regimen of ACE inhibitor, beta-blocker, calcium channel blocker and loop diuretics are potent agents for uncontrolled blood pressure. Though they lowered the blood pressure effectively, chlorthalidone did cause hypokalemia, hypercalcemia, hyperuricemia, hyponatremia, and orthostatic hypotension, so caution is advised. Patients with advanced CKD are often not invited to major clinical trials and so little of their care is vetted with carefully done clinical trials, so when we get this data it deserves to be a Top Story of 2021.
3. Keep on Flozin’ing IgA Subgroup of DAPA CKD in KI
post by Tom Oates
Few things inspired the British philosopher Bertrand Russell more than the problem of induction. Amongst his writings on the topic was this: “The principle of induction, as applied to causation, says that, if A has been found very often accompanied or followed by B, then it is probable that on the next occasion on which A is observed, it will be accompanied or followed by B.” The recent history of nephrology suggests a reasonable substitution for A could be “use of SGLT2 inhibitors in proteinuric kidney disease” and B, “improvement in a hard kidney outcome”. It was perhaps not a surprise therefore when, in April 2021, a pre-specified analysis of the 270 patients with IgA nephropathy enrolled in the Dapa-CKD trial showed that B again followed A. Specifically, the hazard ratio for the primary outcome (sustained decline in eGFR of 50% or more, end-stage kidney disease, or death from a kidney disease-related or cardiovascular cause) was an impressive 0.29 (95% CI 0.12, 0.73); the mean rate of eGFR decline with dapagliflozin was better than placebo (−3.5 and −4.7 mL/min/year respectively); and dapa reduced the urinary ACR by 26% relative to placebo. Purists (and those with financial interests in ongoing trials of novel drugs for IgA nephropathy) have pointed out that this wasn’t a trial designed specifically to examine patients with IgA, and that in an often slowly progressive disease a 2.1 year median follow up time could be extended, but this is another big feather in the cap of the SGLT2 inhibitors in the treatment of proteinuric CKD of any cause.
2. New eGFR Equations: Remove Race in eGFR Equations in NEJM
post by Matthew Sparks @Nephro_Sparks
2021 brought about significant change in how we measure kidney function with estimating equations. No doubt, this story in my opinion should have been #1. Last year the creation of the ASN/NKF national joint task force on reassessing the inclusion of race in diagnosing kidney disease came in as the #9 Top Nephrology Stories of 2020. In September of 2021 the task force released its final report with a simultaneous publication in NEJM. The task force recommended that all eGFR calculations be derived from the 2021 CKD EPI equation without a race variable. The task force also recommended increased use of cystatin C. It is important to emphatically state that race is a socio-political construct and not a biologic or genetic determinant. How race is used in research and medicine is a topic we all should take time to learn and reflect upon. We are now in the process, as individuals and as a field, of doing the hard, and needed, work of eliminating disparities that are long-standing in nephrology; from institutional racism, to social contexts, national policies, to physical contexts. It was refreshing to see equity lifted as a centerpiece of ASN Kidney Week 2021. Let’s all continue this work in 2022 and beyond.
“Scientists have reached general agreement in [recognizing] that mankind is one: that all men [people] belong to the same species, Homo sapiens. The myth of ‘race’ has created an enormous amount of human and social damage. In recent years it has taken a heavy toll in human lives and caused untold suffering. It still prevents the normal development of millions of human beings and deprives [civilization] of the effective co-operation of productive minds.” In “The race question” United Nations Educational, Scientific and Cultural Organization UNESCO 1950 from Mohottige et al CJASN 2021.
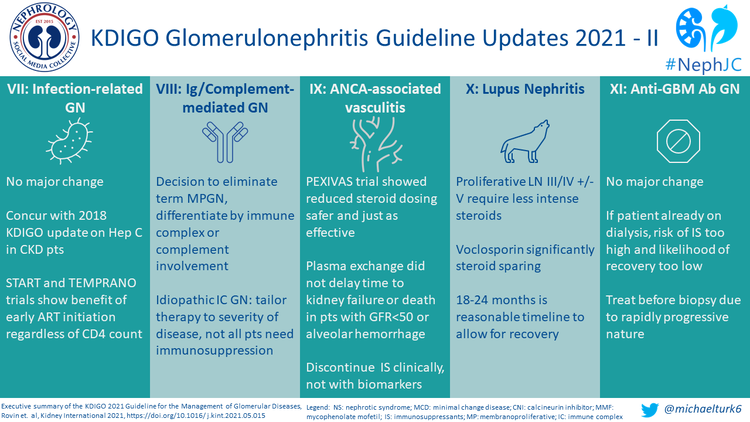
1. KDIGO GN 2021 Update in KI
post by Sudha Mannemuddhu @drM_sudha
Glomerulonephritis (GN) is a complex collection of diseases and sometimes, very difficult to treat. It is always good to have a set of guidelines to evaluate and manage these patients. KDIGO just provided updated guidelines for 2021, and obviously, they have to be ranked number one. So, what’s new? Let’s start with IgA nephropathy-cool calculators- New QxMD calculator to assess with prognosis based on the MEST-C scoring system. It's available for pediatric patients too. RAS inhibitors are still the first line of choice, if proteinuria persists, can consider a 6 month course of steroids. Membranous nephropathy & its unpronounceable antigens- biopsy is not needed for diagnosis in patients that present with nephrotic syndrome and positive Anti-PLA2R antibody. Also, anti-PLA2R antibody levels should be used to guide therapy. Treatment is based on disease severity- Rituximab in moderate to severe risk and Cyclophosphamide & steroids in severe to very severe risk population. Nephrotic Syndrome in Children- music to the ears: 8-12 weeks of steroids are comparable to 24 weeks of steroids. In frequent relapsers, consider switching to steroid-sparing agents. Minimal change disease in adults- No major change here: Biopsy is recommended. Steroids are the first choice unless contraindicated. FSGS in adults- new classification: New 4 classes- primary, secondary, genetic, and undetermined cause (FSGS-UC). For FSGS lesions on biopsy with NS features, likely primary, treat with steroids otherwise evaluate for secondary causes and monitor. Infection-related GN- similar to previous: Early initiation of ART in HIV, irrespective of CD4 counts based on START and TEMPRANO trial. Immunoglobulin/ Complement-mediated GN- stop calling it MPGN: 3 classes- Ig/ immune-complex mediated GN (ICGN), complement-mediated GN, membranoproliferative pattern without immune complexes or complement. Therapy is tailored based on severity and not all patients need immunosuppression. RAS inhibitors rule again as the first line. Anti-Neutrophil cytoplasmic antibodies (ANCA)- associated vasculitis- another melody here: reduced dose steroids are as effective as high dose (PEXIVAS); plasma exchange (PLEX) is not recommended unless there are anti-GBM antibodies. Prefer rituximab unless there is a severe disease (cyclophosphamide). Maintenance therapy should be based on clinical course, not on biomarkers. Lupus Nephritis- more changes to come soon: Induction therapy is similar to 2012 guidelines, with a lower cumulative dose of IV and oral steroids and replacement of NIH cyclophosphamide regimen with Euro-lupus protocol. Newer drugs like Voclosporin (AURORA trial) and Belimumab (BLISS-LN) have shown promising results. Mycophenolate mofetil (MMF) is still the first line for the maintenance regimen. Anti-glomerular basement membrane (Anti-GBM) antibody GN- same guidelines: Treat promptly, even before the biopsy. PLEX is recommended until antibody titers are undetectable. For patients on dialysis, particularly those with >85% crescents, whose risks of immunosuppression may be higher, consider conservative management. Overall, these guidelines recommend the usage of fewer steroids across the spectrum of GN and have clarified and modified several classifications. Well deserved spot at #1 in 2021! Can’t wait to see what 2022 has in store for nephrology.
Post by Matt Sparks, Joel Topf, Michelle Rheault, Tom Oates, Swapnil Hiremath, Sudha Mannemuddhu, Krithika, Mohan, Mohammed Elraggal