The next NephJC will be October 21 at 9pm EDT. We will be discussing the role of troponin in the assessment and management of patients with ESRD.
Playing the foil for this discussion will be two meta analysis from this month's Annals of Internal Medicine.
Summary by JM Topf
Role of Troponin in Patients With Chronic Kidney Disease and Suspected Acute Coronary Syndrome
Stacy SR, Suarez-Cuervo C, Berger Z, Wilson LM, Yeh HC, Bass EB, Michos ED.
PMID: 25111593
Prognostic Value of Cardiac Troponin in Patients With Chronic Kidney Disease Without Suspected Acute Coronary Syndrome
Michos ED, Berger Z, Yeh HC, Suarez-Cuervo C, Wilson LM, Stacy S, Bass EB.
PMID: 25232635
Musical chairs, except, everyone gets a seat.
From the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction (PDF)
Acute coronary syndrome is diagnosed by clinical symptoms, ECG changes and serum cardiac enzymes. Troponin T and I are specific to the cardiac myocyte and have a central role in the diagnosis of ACS. They have a long track record of being both sensitive and specific. Additionally they provide prognostic information adding to their utility in the management of coronary artery disease.
The definition of ACS requires increasing or decreasing levels of troponins. Patients with advanced CKD have the misfortune of having both a terrifyingly high rate of cardiac mortality paired with decreased ability to detect it due to elevated troponin levels.
Note the logarithmic scale on the Y-axis. (Am J Kidney Dis 32[Suppl 3]: S115, 1998) and JASN
Patients with CKD often have persistently elevated troponin levels reducing the specificity of this test. The reason for the increased levels probably has more to do with increased enzyme release from structural heart disease rather than the more conventional definition of decreased clearance. In one study looking at the half-life of troponin I following AMI, found no difference between patients with ESRD and patients with normal renal function.
The accepted definition of AMI in ESRD is,
"A change in troponin level greater than 20% within 9 hours (with at least one value exceeding the 99th percentile)" (PDF)
Troponin in suspected acute coronary syndrome
Methods
With those facts in mind, ale a look at the suspected acute coronary syndrome systemic review. The investigators examined 23 studies literature from 1990 through 2013. They restricted there analysis to studies that evaluated troponin T and/or I in patients with CKD and suspected ACS.They included RCTs and observational studies that included a comparison group.
Outcomes of interest were:
- Sensitivity and specificity for a final clinical diagnosis of ACS
- Positive and negative predictive value for a final clinical diagnosis of ACS
- Differences in ACS management strategies by troponin thresholds
- Differences in all-cause mortality, cardiovascular mortality, and MACEs based on troponin level.
Results
There was tremendous variability in the studies making the results unclear. Regarding diagnostic accuracy they found:
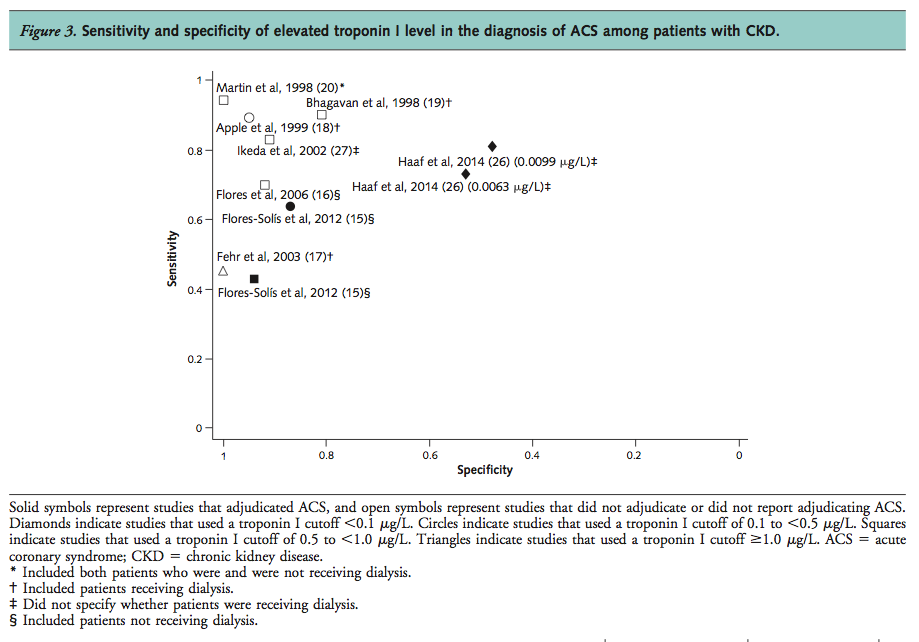
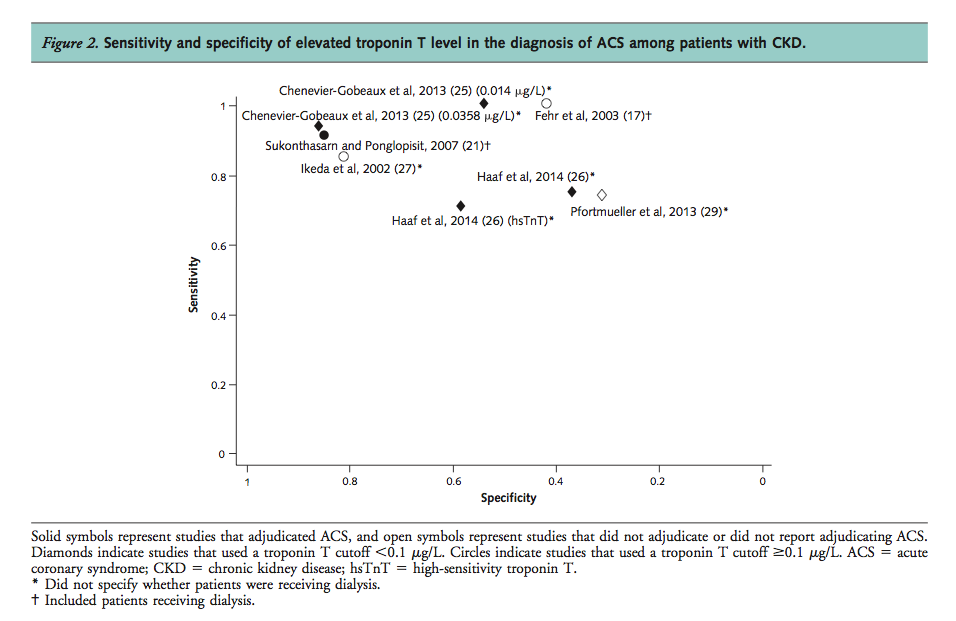
The sensitivity for ACS diagnosis ranged from 71% to 100% for troponin T and from 43% to 94% for troponin I. Specificity ranged from 31% to 86% for troponin T and from 48% to 100% for troponin I. Given heterogeneity of troponin cutoffs and assay manufacturers in these studies, we could not identify a trend relating assay cutoff value to these characteristics.
We found insufficient evidence from 1 study (21) for the diagnostic accuracy of a change in troponin level. The magnitude of change in troponin T level in the first 24 hours after hospitalization did not differ between the control and ACS groups (n=46). Similarly, the rates of change from 0 to 6 and from 6 to 12 hours after hospitalization did not differ between groups.
Read that second paragraph again as you wait for your serial troponins to come back on all of your dialysis patients.
Prognosis was worse with higher Troponin T and I but the strength of evidence was low for both assays.
Conclusion
The conclusion they came to was:
In a systematic review of the evidence, we found low-quality or insufficient evidence for the utility of troponin T and troponin I assays for diagnosis and management of ACS and for the prognostic value of elevated troponin levels for ACS in patients with CKD, except in certain patient subgroups.
There conclusions were limited due to variability in the assays used, definitions of CKD and the cut points for abnormal troponin.
They were unable to find data to support the recommendation of using a 20% change in troponin within 9 hours to diagnose AMI in ESRD.
Troponin in CKD patients without suspected acute coronary syndrome
The unsuspected acute coronary syndrome systemic review begins with this sentence, a critical one to keep in mind for this subject:
However, elevated troponin levels may be due to cardiac injury associated with chronic structural heart disease rather than acute ischemia, especially when levels do not change
Methods
This study did a systemic review of the prognostic implications of elevated troponinsin CKD in patients without any symptoms of ACS. They looked at mortality and major adverse coronary events (MACE). They found 98 studies. Follow-up ranged from 30 days to 5 years.
Results
Conclusion
Money quote:
...elevated troponin levels among these patients are not spurious but portend a worse prognosis...
Too often I see residents dismiss an elevated troponin in a dialysis patient, even though an elevated troponin does not establish a diagnosis as it is used in patients without kidney disease it does provide information about the patients cardiac risk.



![Note the logarithmic scale on the Y-axis. (Am J Kidney Dis 32[Suppl 3]: S115, 1998) and JASN](https://images.squarespace-cdn.com/content/v1/535bcb2fe4b05fe61b320c51/1413561922506-J8GNPAU88DF4PQW9KV9H/kck_f6.gif)