#NephJC Chat
Tuesday Nov 28 9 pm Eastern
Wednesday Nov 29 8 pm GMT, 12 noon Pacific
N Engl J Med. 2017 Nov 12. doi: 10.1056/NEJMoa1710933. [Epub ahead of print]
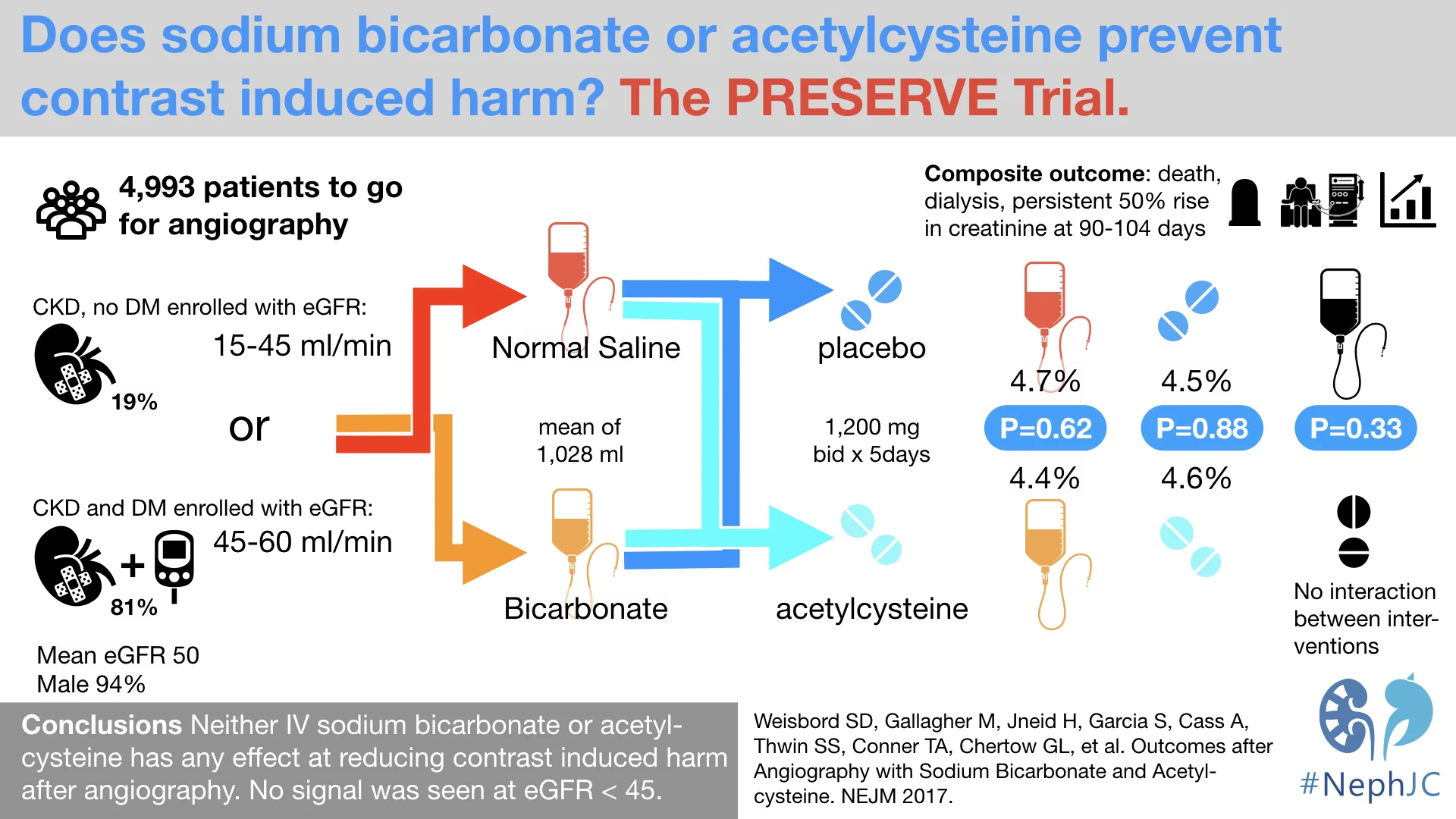
Outcomes after Angiography with Sodium Bicarbonate and Acetylcysteine.
Weisbord SD, Gallagher M, Jneid H, Garcia S, Cass A, Thwin SS, Conner TA, Chertow GM, Bhatt DL, Shunk K, Parikh CR, McFalls EO, Brophy M, Ferguson R, Wu H, Androsenko M, Myles J, Kaufman J, Palevsky PM; PRESERVE Trial Group.
PMID: 29130810 Full Text at NEJM
Introduction
Imaging with iodinated contrast is one of the few scenarios, where we know the exact time and place where kidney injury can happen. Given that it is usually elective, that has lead to a bunch of prophylactic agents being employed to protect the kidney. The oldest and brightest of these is volume expansion. There are two broad schools of thought about the pathophysiology of contrast nephropathy, one being concentration and blockage of the tubules by the the viscous contrast material, and the other being tubular damage from reactive oxygen species. The latter theory is what birthed the trial in 2000 with n-acetyl cysteine (NAC), which helps regenerate glutathione, one of the most well studied endogenous antioxidants. This trial by Tepel showed a dramatic reduction of acute kidney injury (AKI), though the promise was not upheld in subsequent RCTs, which were a curious mix of positivity and negativity. A similar theme played out after a small positive RCT of isotonic sodium bicarbonate for the prevention contrast nephropathy followed by a mixture of positive and negative trials. Meta-analyses (note the plural) followed, and given the heterogeneity, some were positive and some were negative - with at times the somewhat tragicomic stat of the number of meta-analyses approaching the number of RCTs. Into this morass, Drs Weisbord and Palevsky designed a large - yes, really large - RCT, this time testing these two interventions in a 2x2 factorial design, with a clinically relevant outcome, not just changes in creatinine.
The Study
Methods
Funding: The trial was funded by the Veterans Affairs, and the NHMRC (Australia) and conducted by the VA along with the George Institute
Population:
Inclusion Criteria:
Patients undergoing coronary or non-coronary angiography
GFR 15 - 44 ml/min/1.73 m^2 with or without diabetes
GFR 45 - 59 ml/min/1.73 m^2 if they also had diabetes
Exclusion criteria:
Emergency angiographies
Patients with decompensated heart failure, shock
Patients with acute fluctuations in kidney function
Others (pregnancies, inability to give consent, etc)
Interventions
Bicarb vs Saline Comparison
IV 1.26% sodium bicarbonate (150 mmol per liter) or IV 0.9% sodium chloride (154 mmol per liter) in matched 1-liter bags, given as:
1 to 3 ml per kg of body weight per hour during a period of 1 to 12 hours for a total volume of 3 to 12 ml per kg before angiography,
1 to 1.5 ml per kg per hour during angiography,
and 1 to 3 ml per kg per hour during a period of 2 to 12 hours post angiography
Thus a total volume of 6 to 12 ml per kg associated with angiography.
Within these specific parameters, the providers at trial sites determined the timing of initiation, duration, and rate of fluid administration. For BMI > 30, the fluid-administration rates was capped using a weight of 125 kg.
NAC vs placebo comparison
1200 mg of oral NAC or matched placebo approximately 1 hour before angiography and again 1 hour after angiography.
Continued as 1200 mg of NAC or matched placebo twice daily for the following 4 days for a total of 10 doses.
Outcomes
The primary end point was a composite of
Death
Need for dialysis, or
Persistent impairment in kidney function: a persistent increase of at least 50% from baseline in the serum creatinine level at 90 to 104 days after angiography and confirmed at subsequent testing within 14 days
Analytic Plan
This was a standard, modified, intention to treat analysis
For sample size, they estimated that 7680 patients would provide a power of 90% to detect a decrease in the rate of the primary end point from 8.7% to 6.5% for each trial intervention. For comparison of numbers, the original NAC RCT had 83 patients, and the first bicarb RCT had 119 patients.
An interim analysis was planned when ~ 50% of patients would have reached 90 day follow up.
Results
The trial was halted for futility at the interim analysis, with just over 5000 of the ~ 8000 patients enrolled.
Of the 5000 patients, roughly 2,500 each received each of the four interventions.
Figure 1 from Weisbord et al, NEJM 2017
About 700 were enrolled by the George Institute, and the remaining ~ 4,300 by the Veterans Affairs, hence ~94% were men. The average age was about 70 years, 81% were diabetic, and the mean baseline GFR was about 50 (more details in Table 1). Most patients (90.5%) underwent coronary angiogram, with a mean volume of contrast of about 85 ml, and just under a third (28.5%) also had a percutaneous coronary intervention. The adherence to the interventions was fairly typical, and the bicarb administration did result in a higher urinary pH (6.7 vs 6.0 in saline).
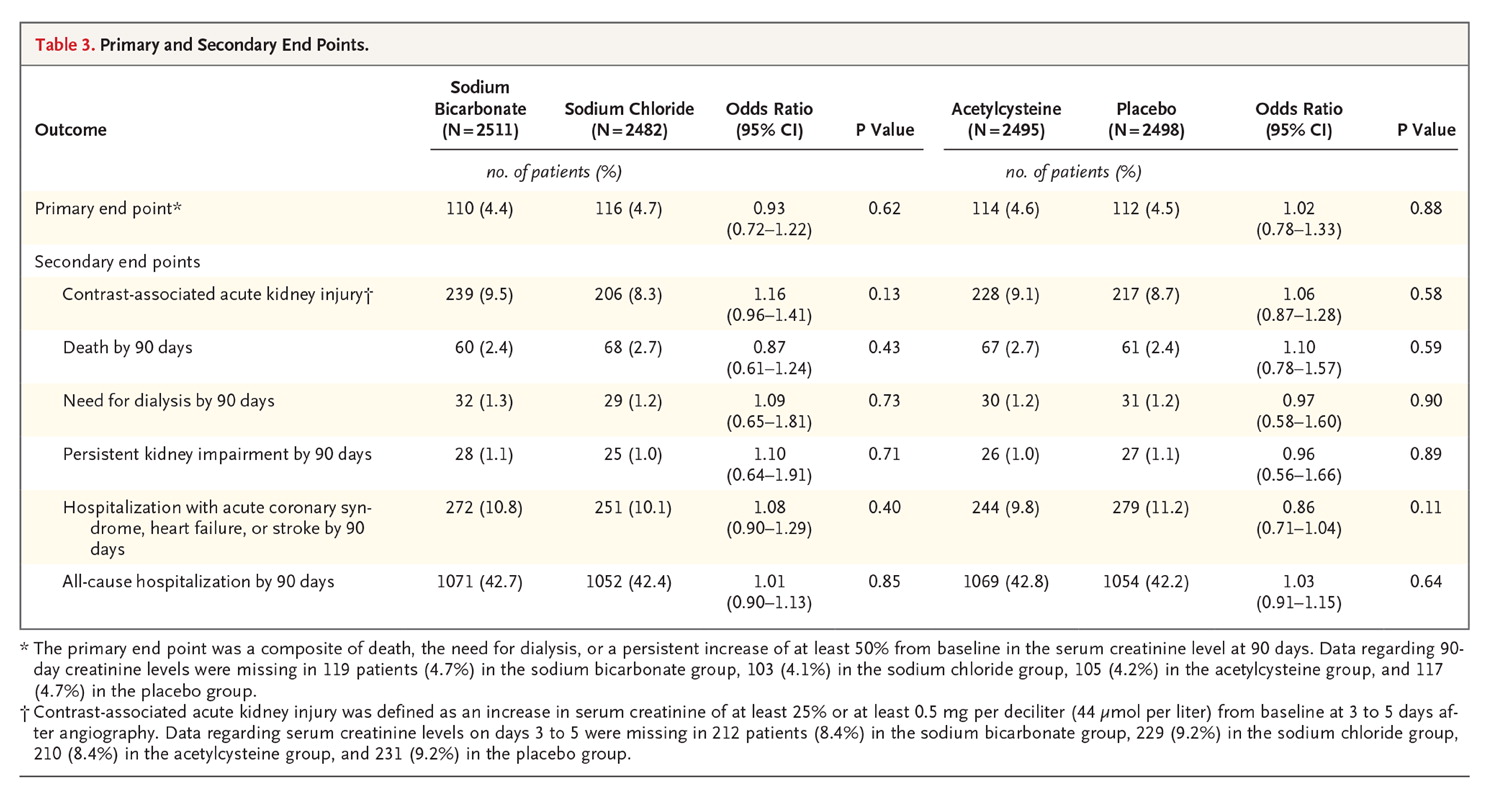
And the outcomes? About 5% in all 4 groups developed the outcome, see below from table 3. Even if the trial had kept on enrolling patients, with this event rate and difference between groups, the conditional power would be 5.2% at an alpha level of 0.024 and 11.3% at an alpha level of 0.048 if all new primary events occurred at the observed rates only in the control groups. Hence the DSMB recommended halting the study, appropriately.
Table 3 from Weisbord et al, NEJM 2017
There was no interaction between bicarb and NAC either (p = 0.46). Nor was there any signal in the secondary outcomes (see table 3 above), or the subgroup analysis (figure 2 below).
Figure 2 from Weisbord et al, NEJM 2017
If one is curious about that p = 0.02 for coronary vs non-coronary angiography, this should set that straight:
Discussion
These results seem quite unequivocal - many of us were already quite convinced that NAC in contrast AKI prevention is of no merit (especially after the ACT trial), however, a recent AHRQ-funded systematic review had concluded otherwise (due to methodological limitations). An often heard refrain on NAC also is: 'it doesn't do any harm, so why not use it?' Hence this definitive RCT hopefully puts those feelings to rest.
For bicarb - balanced solutions in AKI, outside the contrast AKI field, have made a comeback and are still being studied (see #NephJC discussion of one of those RCTs here). However, again, in the setting of contrast administration, there seems no difference between using bicarb-based solutions or plain old saline.
One could only ask, why did this medical reversal take so long?
But there's more: now we don't use NAC, we use bicarb or saline interchangeably, but do we need any IV volume expansion at all? Could oral salt/water be just as good? What about giving nothing at all - as a recent RCT suggested? And did we forget about using the left ventricular end diastolic pressure (LVEDP) to guide volume - as we discussed from the POSEIDON trial? Does contrast AKI even exists (but we did that on NephJC, lets try not to go there again, please)? Bring these questions and more to the #NephJC chat.
Summary by Swapnil Hiremath, Ottawa