Akshaya Jayachandran, NephJC intern was inspired by John Green’s Everything is Tuberculosis to write the following poem.
#NephJC Summer Bookclub: Everything is Tuberculosis by John Green
The summer book club started in 2015, with one of the best books we have done in book club, Atul Gawande's Being Mortal. I think it should be required reading for all physicians. So now, in 2025, it is the NephJC Summer Book’s tenth anniversary (which represents our eleventh book). The history has been rich:
Summer Book Club 2024. The Covenant of Water
NephJC Summer Book Club
Summer Book Club 2023. How Medicine Works and When It Doesn't by F. Perry Wilson
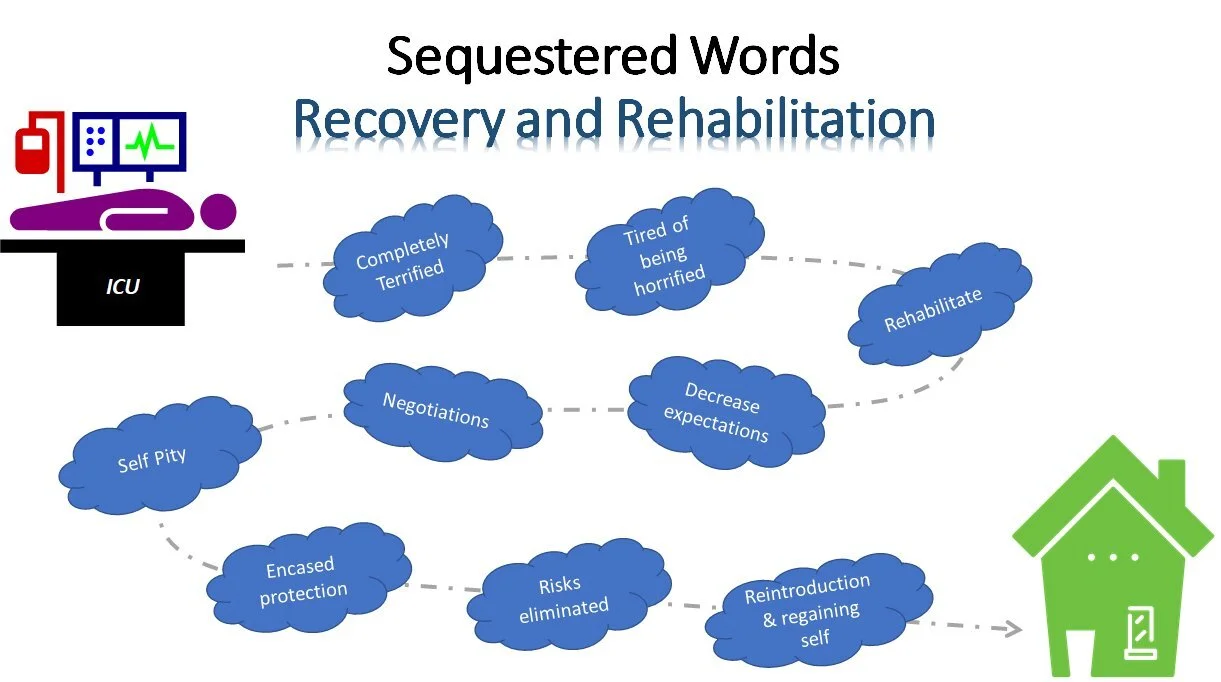
In Shock, some illustration by Sudha Mannemuddhu
In Shock, Chapter 8: Censors of Light
In Shock, Chapter 2: A Hollowness
In Shock, Chapter 6: Shifting Frames
In Shock, Chapter 1: Bled White
Rana Awdish's In Shock
NephJC Summer Bookclub: Doctor (Object Lesson)
Law 2. Normals teach us rules; Outliers teach us laws
I search for patterns, always have. The logic of symptomatology is Glorious. I suspect this character trait is common in nephrologists. But revelling in the symptoms and signs that lead to a diagnosis and the investigative algorithm that refines the differential into the definite, has meant that I focus on what Siddhartha terms “inliers”. As I seek to make a patient “fit” my pre-conceived pathogenic model, I run the risk of missing a deeper truth. Brahe concentrated on the inliers and modelled the movement of the planets into concentric circles, frustrated that Mars wouldn’t fit this model. Kepler used the movement of the outlier, Mars, to reveal that all the planets orbit the sun in concentric ellipses. By concentrating on the range of normalcy we can only create rules, whereas “outliers” allow access to deeper laws.
Each outlier represents an opportunity to refine our understanding of illness. Asking why one patient in a thousand has responded to a drug, can reveal new disease pathways. David Solit used this approach to investigate why one woman’s advanced bladder cancer had a spectacular response to everolimus, while the drug appeared ineffective for the cohort as a whole. Sequencing that woman’s tumour showed multiple mutations, most interestingly in TSC1 and NF2, suggesting that these genes modulated the response to everolimus. The group went on to sequenced the same genes in the larger cohort and were able to segregate the group into responders and non-responders by the mutation in the TSC1 gene. In doing so they opened up new lines of enquiry and broadened the understanding of everolimus, bladder cancer, tuberous sclerosis and neurofibromatosis.
Through seeking to understand the outlier they opened up a deeper understanding of disease.
Now that case reports have fallen out of fashion, becoming almost impossible to publish and dismissed as anecdote, where are we to find our outliers? One option is to conduct “outlier rounds” as Siddhartha suggests, another is to seek out case report posters at conferences. But a further powerful option is to maintain an open dialogue with colleagues, whether in person or online, to tell our stories and to ask the deeper questions.
Cathy Quinlain